Pancreatic Hormones
Pancreatic Hormones
Pancreas is both exocrine and endocrine gland. The exocrinal part secretes pancreatic fluid into the duodenum after a meal. The endocrinal part secretes various types of hormones. These are produced by a specialized tissue in the pancreas and then released to the capillary system and reached the liver by the portal venous circulation. The specialized tissue is called islets of Langerhans. Islets of Langerhans represent approximately 1-2 % of the pancreas. Three types of cells are regonized in these islets.
- A cells – producing glucagon (25% of all islet cells).
- B cells – producing insulin (60% of all islet cells).
- D cells – producing somatostatin (10% of all islet cells).
- F cells – producing panceratic polypeptide (5% of all islet cells).
Islets of Langerhans play a crucial role in carbohydrate metabolism and so in a plasma glucose concentration. It involves:
- Glycolysis – the anaerobic conversion of glucose to lactate. Occurs in the red blood cells, renal medulla and sceletal muscles.
- Glycogenesis – the synthesis of glycogen from glucose. Glucose is stored ( in liver, muscle) in the form of glycogen and this serves to maintain a constant plasma glucose concentration.
- Glycogenolysis – the breakdown of glycogen to glucose.
- Gluconeogenesis – the production of glucose from non-sugar molecules (amino acids, lactate, glycerol)
- Lipolysis – the breakdown of triacylglycerols into glycerol and free fatty acids.
- Lipogenesis – the synthesis of triacylglycerols.
Function
- Pancreatic hormones are responsible for storage of fat and glucose, as glycogen, after meal.
- Enables the mobilisation of energy reserves as a result of food deprivation, stress, physical activity.
- Maintain the constant plasma glucose concentration.
- Promote growth.
Pancreatic hormone
Insulin
Structure
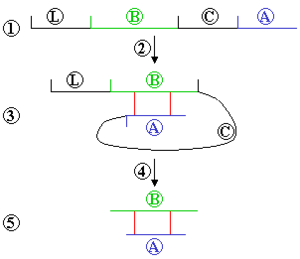
Insulin is a peptide consisting of an α-chain 21 amino acids long linked to a 30 amino acid β-chain via two disulfide bridges. The precursor to insulin is preproinsulin, which contains a signal sequence that is further removed in the endoplasmic reticulum converting the precursor into its prohormone referred to as proinsulin. Proinsulin is converted into insulin after removal of a C-peptide from the prohormone.
The insulin receptor consists of two extracellular α-subunits and two transmembraneous β-subunits. When insulin is near the receptor, it binds to the α-subunits of the receptor. This binding leads to the autophosphorylation of the β-subunits of the insulin receptor. These β-subunits then act as receptor tyrosine kinases that phosphorylate insulin receptor subunits. The signal then travels downstream to intracellular proteins.
Regulation
Insuline is mainly secreted in a response to increases in the blood levels of glucose. Higher level of glucose cause that glucose enter the B cells and is converted to a glucose-6-phosphate. This creates the cytosolic ATP and leads to a closure of ATP-gated channels and then to depolarization. Depolarization causes an opening of voltage-gated channels and the level of cytosolic rises and initiates an exocytosis of insulin and re-openning of channels. Insulin secretion is stimulated during digestion via acetylcholin (vagus nerve), gastrin, sekretin. Certain amino acids as a arginin and leucin also stimulate secretion as well as free fatty acids and some steriod hormones. The secretion is inhibited via epinephrine and norepinephrine. These are activated when hypoglycemia is detected by central chemoreceptors.
channels and then to depolarization. Depolarization causes an opening of voltage-gated channels and the level of cytosolic rises and initiates an exocytosis of insulin and re-openning of channels. Insulin secretion is stimulated during digestion via acetylcholin (vagus nerve), gastrin, sekretin. Certain amino acids as a arginin and leucin also stimulate secretion as well as free fatty acids and some steriod hormones. The secretion is inhibited via epinephrine and norepinephrine. These are activated when hypoglycemia is detected by central chemoreceptors.
channels and then to depolarization. Depolarization causes an opening of voltage-gated channels and the level of cytosolic rises and initiates an exocytosis of insulin and re-openning of channels. Insulin secretion is stimulated during digestion via acetylcholin (vagus nerve), gastrin, sekretin. Certain amino acids as a arginin and leucin also stimulate secretion as well as free fatty acids and some steriod hormones. The secretion is inhibited via epinephrine and norepinephrine. These are activated when hypoglycemia is detected by central chemoreceptors.
channels and the level of cytosolic rises and initiates an exocytosis of insulin and re-openning of channels. Insulin secretion is stimulated during digestion via acetylcholin (vagus nerve), gastrin, sekretin. Certain amino acids as a arginin and leucin also stimulate secretion as well as free fatty acids and some steriod hormones. The secretion is inhibited via epinephrine and norepinephrine. These are activated when hypoglycemia is detected by central chemoreceptors.
Function
Insulin has anabolic and lipogenic effects. It promotes the storage of glucose in the liver and also activates enzymes to promote glycolysis and glycogenesis. In addition, it promotes the uptake and storage of amino acids in the form of proteins and promotes growth. Insulin also increases the amount of GLUT-4. (Glucose transporters in skeletal myocytes. So that glucose can enter. Glucose can enter the cell in two different ways. One is with sodium as a secondary active transport and the other one is through glucose transports, facilitated diffusion.)
Glucagon
Glucagon is a peptide derived from proglucagon (glicentin). Glucagon secretion is stimulated by amino acids, arginin and alanin, from digested proteins. And also by hypoglycemia as a result of physical exercise. And sympathic impulses. The secretion is inhibited by glucose, somatostatin and high plasma concetrations of free fatty acids.
Function
Glucagon mainly antagonise insulin. The signal from glucagon receptor is spread via cAMP. Glucagon increases glycogenolysis in the liver, stimulates gluconeogenesis from lactate, protein degradation and lipolysis. Its main role is to maintain the normal blood glucose level between meals to ensure a constant energy supply.
Somatostatin
Somatostatin is released in response to higher plasma concentrations of glucose and arginine. Through paracrine pathways inhibits the release of insulin and also the secretion of glucagon. During the deficiency of glucose this process does not occur due to the release of catecholamines that inhibit the secretion of somatostatin.
Diabetes Mellitus
There are two types recognized. One type of diabetes mellitus is insulin-dependent, type-1, which is caused by insulin deficiency. Another type is non-insulin-dependent, type 2, which is caused by a shortage of insulin receptors. In both cases the level of glucose in blood is increased and this leads to glycosuria, polyuria and polydipsia. Since lipolysis is no longer inhibited, fatty acids are liberated in a large quantities. Fatty acids can be used as a source of energy, although, this leads to formation of acetoacetic acids and acetone (ketosis). As a result of so many fatty acids the liver begins to store triacylglycerols which leads to the development of fatty liver.
Links
Related articles
Bibliography
- SILBERNAGL,. Color Atlas of Physiology. 5. edition. 2001. ISBN 3-13-545005-8.
- GANONG,. Přehled lékařské fyziologie. 1. edition. 1995. ISBN 80-85787-36-9.