Immunological development of the child: Difference between revisions
(Created page with "The immune system is a collection of mechanisms that maintain the integrity of the organism. It is a complex system of cells and molecules that have the ability to recogni...") |
m (Checked by the editor, grammar has NOT been corrected) |
||
| (One intermediate revision by one other user not shown) | |||
| Line 1: | Line 1: | ||
[[The immune system]] is a collection of mechanisms that maintain the integrity of the organism. It is a complex system of cells and molecules that have the ability to recognize and eliminate both foreign and own potentially harmful structures. [[Immunocompetent cells]] arise from a common stem cell in the bone marrow and then mature and differentiate in the central (primary) lymphatic organs (bone marrow, thymus,...). Immune reactions take place in peripheral (secondary) lymphatic organs, which are either anatomically defined structures (lymph nodes, spleen) or functional units ([[Mucosal immune system|mucosal]] and [[Skin immune system|skin immune system,]] the immune system of individual organs). Disorders in the structure or function of the immune system can cause increased susceptibility to infections, the development of autoimmune diseases, allergies or tumors. | [[The immune system]] is a collection of mechanisms that maintain the integrity of the organism. It is a complex system of cells and molecules that have the ability to recognize and eliminate both foreign and own potentially harmful structures. [[Immunocompetent cells]] arise from a common stem cell in the bone marrow and then mature and differentiate in the central (primary) lymphatic organs (bone marrow, thymus,...). Immune reactions take place in peripheral (secondary) lymphatic organs, which are either anatomically defined structures (lymph nodes, spleen) or functional units ([[Mucosal immune system|mucosal]] and [[Skin immune system|skin immune system,]] the immune system of individual organs). Disorders in the structure or function of the immune system can cause increased susceptibility to infections, the development of autoimmune diseases, allergies or tumors.<ref name="KlinPed2012">{{Cite| type = book| surname1 = Lebl| name1 = J| surname2 = Janda| name2 = J| surname3 = Pohunek| name3 = P| colective = yes| title = Klinická pediatrie| edition = 1| publisher = Galén| year = 2012| pages = 223| range = 698| isbn = 978-80-7262-772-1}}</ref> | ||
==Structure of the immune system== | ==Structure of the immune system== | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 32: | Line 32: | ||
* '''Lymphoid cell line''': [[T cells|T-cells]] (mediate a specific immune response), [[B - Lymphocytes|B-cells]] (provide specific antibody immunity), [[NK cells]] (cytotoxic cells of non-specific immunity) | * '''Lymphoid cell line''': [[T cells|T-cells]] (mediate a specific immune response), [[B - Lymphocytes|B-cells]] (provide specific antibody immunity), [[NK cells]] (cytotoxic cells of non-specific immunity) | ||
* '''Myeloid cell line''': [[Monocyte|monocytes]] - [[macrophages]] ([[Antigen-presenting cells|antigen-presenting phagocytic cells]]), [[dendritic cells]], [[neutrophilic granulocytes]] (phagocytic cells of an early inflammatory response), [[Basophil Granulocyte|basophil granulocytes]] (peripheral blood cells participating in the inflammatory response), [[Eosinophil granulocyte|eosinophil granulocytes]] (cells participating in the hypersensitivity reaction and antiparasitic defense), [[mast cells]] ([[Immunopathological reaction type I|type I hypersensitivity reaction cells]]) | * '''Myeloid cell line''': [[Monocyte|monocytes]] - [[macrophages]] ([[Antigen-presenting cells|antigen-presenting phagocytic cells]]), [[dendritic cells]], [[neutrophilic granulocytes]] (phagocytic cells of an early inflammatory response), [[Basophil Granulocyte|basophil granulocytes]] (peripheral blood cells participating in the inflammatory response), [[Eosinophil granulocyte|eosinophil granulocytes]] (cells participating in the hypersensitivity reaction and antiparasitic defense), [[mast cells]] ([[Immunopathological reaction type I|type I hypersensitivity reaction cells]])<ref>http://fvl.vfu.cz/export/sekce_ustavy/mikrobiologie/imunologie/Prednasky/02_8_bunky_organy_bariery.pdf</ref> | ||
[[File:Cells of the immune system.jpg|thumb|310x310px|Cells of the immune system]] | [[File:Cells of the immune system.jpg|thumb|310x310px|Cells of the immune system]] | ||
| Line 43: | Line 43: | ||
The newborn has a functional immune system (which is capable of both humoral and cellular immune responses) and in the first months of life is additionally protected by transplacentally transferred [[IgG|IgG antibodies]] from the mother. The IgG transfer occurs from the 22nd gestational week thanks to specific Fc-receptors in the [[placenta]]. The infant is further protected by the mother's IgA obtained from breast milk, however, these IgA protect against pathogens only in the area of the digestive tract and do not enter the newborn's bloodstream. | The newborn has a functional immune system (which is capable of both humoral and cellular immune responses) and in the first months of life is additionally protected by transplacentally transferred [[IgG|IgG antibodies]] from the mother. The IgG transfer occurs from the 22nd gestational week thanks to specific Fc-receptors in the [[placenta]]. The infant is further protected by the mother's IgA obtained from breast milk, however, these IgA protect against pathogens only in the area of the digestive tract and do not enter the newborn's bloodstream. | ||
The lowest level of immunoglobulins in the infant's serum is around the 4th to 6th month of age, because during this period passively acquired maternal [[IgG]] has already broken down and the endogenous synthesis of [[Immunoglobulin family|immunoglobulins]] is not yet sufficient. It is during this period where the clinical manifestations of humoral immunodeficiencies occur. | The lowest level of immunoglobulins in the infant's serum is around the 4th to 6th month of age, because during this period passively acquired maternal [[IgG]] has already broken down and the endogenous synthesis of [[Immunoglobulin family|immunoglobulins]] is not yet sufficient. It is during this period where the clinical manifestations of humoral immunodeficiencies occur.<ref name="kddl">http://www.vfn.cz/pracoviste/kliniky-a-oddeleni/klinika-detskeho-a-dorostoveho-lekarstvi/</ref><ref>http://jeeves.mmg.uci.edu/immunology/CoreNotes/Chap17.pdf</ref> | ||
==T-cell development== | ==T-cell development== | ||
| Line 52: | Line 52: | ||
* '''Negative selection''' – thymocytes with high expression of TCR reacting with self-peptides presented with HLA I or II on thymic macrophages → induction of [[apoptosis]] → '''deletion of autoreactive clones'''. | * '''Negative selection''' – thymocytes with high expression of TCR reacting with self-peptides presented with HLA I or II on thymic macrophages → induction of [[apoptosis]] → '''deletion of autoreactive clones'''. | ||
T-cells then migrate to the secondary lymphatic organs. | T-cells then migrate to the secondary lymphatic organs.<ref name="kddl"/> | ||
==B-cell development== | ==B-cell development== | ||
| Line 76: | Line 76: | ||
* The contact of T-cells and B-cells is enabled via CD28 + CD80/86, CD40L + CD40 and leads to the multiplication of B-cells and differentiation into: | * The contact of T-cells and B-cells is enabled via CD28 + CD80/86, CD40L + CD40 and leads to the multiplication of B-cells and differentiation into: | ||
** '''Plasma cells''' → production of antigen-specific IgM (low affinity, blocking infection), IgM + Ag = immune complexes → binding to DC in nodes; | ** '''Plasma cells''' → production of antigen-specific IgM (low affinity, blocking infection), IgM + Ag = immune complexes → binding to DC in nodes; | ||
** '''Memory cells''' - "switch" genes for Ig to produce [[IgG]], [[IgA]] or [[IgE and IgD|IgE]]. | ** '''Memory cells''' - "switch" genes for Ig to produce [[IgG]], [[IgA]] or [[IgE and IgD|IgE]]. <ref name="jcu">eamos.pf.jcu.cz/amos/kpk/externi/kpk_2816/8.ppt</ref><ref name="kddl"/> | ||
; Secondary phase of the antibody response (secondary response) | ; Secondary phase of the antibody response (secondary response) | ||
| Line 85: | Line 85: | ||
** [[Antibody class switching]] - IgG, IgA, IgE; | ** [[Antibody class switching]] - IgG, IgA, IgE; | ||
** The formation of plasma and memory cells with a higher affinity to Ag (somatic mutations of Ig genes increase the affinity of antibodies). | ** The formation of plasma and memory cells with a higher affinity to Ag (somatic mutations of Ig genes increase the affinity of antibodies). | ||
* Secondary response result = Ig with higher affinity to Ag able to [[Complement activation|activate complement]] and [[Opsonization|opsonize]] (IgG+FcR). | * Secondary response result = Ig with higher affinity to Ag able to [[Complement activation|activate complement]] and [[Opsonization|opsonize]] (IgG+FcR). <ref name="kddl"/> | ||
Primary and secondary responses to each other during typical infections immediately follow and lead to the formation of memory cells. In case of repeated infection (subsequent encounter with Ag): | Primary and secondary responses to each other during typical infections immediately follow and lead to the formation of memory cells. In case of repeated infection (subsequent encounter with Ag): | ||
* The level of Ig persists - immediate suppression of infection. | * The level of Ig persists - immediate suppression of infection. | ||
* Memory cells are rapidly activated to produce high-affinity Ig of different isotypes . | * Memory cells are rapidly activated to produce high-affinity Ig of different isotypes . <ref name="jcu"/> | ||
* Terminal maturation into plasma cells : | * Terminal maturation into plasma cells : | ||
| Line 101: | Line 101: | ||
=== B-lymphocytes === | === B-lymphocytes === | ||
There is a higher number of B-lymphocytes in the umbilical cord blood. However, they do not yet form the entire spectrum of [[Antibody|immunoglobulins]] (Ig). After stimulation by [[Antigen|antigens]] (Ag) from the external environment, IgM is first formed (this ability is also present in immature B-lymphocytes). The total Ig level is lowest around 3 to 4 months of age. The ability to form Ig against protein Ag is present from birth, but the ability to form Ig against polysaccharide Ag is non-efficient until 2 years of age (polysaccharide vaccine is not suitable, rather a conjugate vaccine must be used, e.g. against ''[[Haemophilus influenzae|Haemophilus influenzae type B]]''). The newborn is more susceptible to '''G- infection''' because the lack of IgM (= [[Opsonin|opsonins]] ) causes imperfect phagocytosis of polymorphonuclears. The maternal [[IgG|IgGs]] work as opsonins for most '''G+ bacteria''', specific IgGs are sufficient against common virus infections. Premature infants have less maternal IgG and therefore lower opsonization activity for all types of microorganisms. | There is a higher number of B-lymphocytes in the umbilical cord blood. However, they do not yet form the entire spectrum of [[Antibody|immunoglobulins]] (Ig). After stimulation by [[Antigen|antigens]] (Ag) from the external environment, IgM is first formed (this ability is also present in immature B-lymphocytes). The total Ig level is lowest around 3 to 4 months of age. The ability to form Ig against protein Ag is present from birth, but the ability to form Ig against polysaccharide Ag is non-efficient until 2 years of age (polysaccharide vaccine is not suitable, rather a conjugate vaccine must be used, e.g. against ''[[Haemophilus influenzae|Haemophilus influenzae type B]]''). The newborn is more susceptible to '''G- infection''' because the lack of IgM (= [[Opsonin|opsonins]] ) causes imperfect phagocytosis of polymorphonuclears. The maternal [[IgG|IgGs]] work as opsonins for most '''G+ bacteria''', specific IgGs are sufficient against common virus infections. Premature infants have less maternal IgG and therefore lower opsonization activity for all types of microorganisms.<ref name="kddl"/> | ||
==Lymphatic organs development== | ==Lymphatic organs development== | ||
| Line 108: | Line 108: | ||
* '''Peripheral lymphatic tissues''' - adult size up to 6 years of age, larger in prepubertal period, then involution. | * '''Peripheral lymphatic tissues''' - adult size up to 6 years of age, larger in prepubertal period, then involution. | ||
* '''[[Spleen]]''' - gradually grows into adulthood. | * '''[[Spleen]]''' - gradually grows into adulthood. | ||
* '''Peyer's patches''' - grow gradually, are largest during adolescence. | * '''Peyer's patches''' - grow gradually, are largest during adolescence. <ref name="kddl"/> | ||
==Links== | ==Links== | ||
===Related articles=== | ===Related articles=== | ||
| Line 119: | Line 118: | ||
===References=== | ===References=== | ||
<references /> | |||
Latest revision as of 00:01, 3 February 2023
The immune system is a collection of mechanisms that maintain the integrity of the organism. It is a complex system of cells and molecules that have the ability to recognize and eliminate both foreign and own potentially harmful structures. Immunocompetent cells arise from a common stem cell in the bone marrow and then mature and differentiate in the central (primary) lymphatic organs (bone marrow, thymus,...). Immune reactions take place in peripheral (secondary) lymphatic organs, which are either anatomically defined structures (lymph nodes, spleen) or functional units (mucosal and skin immune system, the immune system of individual organs). Disorders in the structure or function of the immune system can cause increased susceptibility to infections, the development of autoimmune diseases, allergies or tumors.[1]
Structure of the immune system[edit | edit source]
| Innate immunity
(also antigenically non-specific, congenital, non-adaptive ) |
Cell-mediated | Phagocytes |
| Macrophages | ||
| NK-cells | ||
| Humoral | Complement | |
| Interferons (IFN) | ||
| Specific immunity
(also acquired, adaptive) |
Cell-mediated | T-cells |
| Humoral | B-cells → antibodies (Ig) |
- professional phagocytes: polymorphonuclear leukocytes (neutrophils) and monocytes-macrophages;
- macrophages – arise from monocytes by entering tissues, They have diffrent forms with different name in various tissues (lymph nodes = histiocytes; skin and mucous membranes = Langerhans cells; CNS = microglia; liver = Kupffer cells; kidneys = intraglomerular mesangial cells; bones = osteoclasts, etc…);
- NK-cells ( natural killers ) – cytotoxic lymphocytes that are able to quickly kill virus-infected cells and some tumor cells.
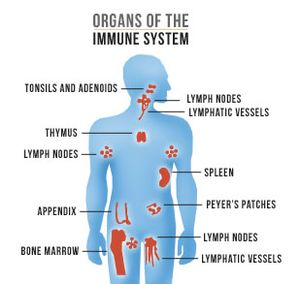
Organs of the immune system[edit | edit source]
- thymus, bone marrow, lymph nodes, spleen, tonsills, Peyer's patches in intestine, apendix
Cells of the immune system[edit | edit source]
- Lymphoid cell line: T-cells (mediate a specific immune response), B-cells (provide specific antibody immunity), NK cells (cytotoxic cells of non-specific immunity)
- Myeloid cell line: monocytes - macrophages (antigen-presenting phagocytic cells), dendritic cells, neutrophilic granulocytes (phagocytic cells of an early inflammatory response), basophil granulocytes (peripheral blood cells participating in the inflammatory response), eosinophil granulocytes (cells participating in the hypersensitivity reaction and antiparasitic defense), mast cells (type I hypersensitivity reaction cells)[2]
Development of the immune system[edit | edit source]
The development of the immune system begins before birth and continues throughout life. Cells of the immune system are developed from hematopoietic stem cells, which are capable of unlimited mitotic division.
In the 3rd week of gestation, a pluripotent hematopoietic stem cell is formed in the yolk sac, which travels in the 5th week of gestation to the fetal liver (the 1st hematopoietic organ of the embryo) and temporarily also to the spleen. From the liver in 8.-11. week of gestation, stem cells are seeded by embryonic circulation into the bone marrow, thymus, spleen and lymph nodes. After birth, the bone marrow is the only hematopoietic organ.
The newborn has a functional immune system (which is capable of both humoral and cellular immune responses) and in the first months of life is additionally protected by transplacentally transferred IgG antibodies from the mother. The IgG transfer occurs from the 22nd gestational week thanks to specific Fc-receptors in the placenta. The infant is further protected by the mother's IgA obtained from breast milk, however, these IgA protect against pathogens only in the area of the digestive tract and do not enter the newborn's bloodstream.
The lowest level of immunoglobulins in the infant's serum is around the 4th to 6th month of age, because during this period passively acquired maternal IgG has already broken down and the endogenous synthesis of immunoglobulins is not yet sufficient. It is during this period where the clinical manifestations of humoral immunodeficiencies occur.[3][4]
T-cell development[edit | edit source]
The thymus is populated by T-cell precursors from the fetal liver ("pro-T cells"). In the thymus occurs the crucial evolution of TCRs ( T-cell receptors ) and, due to random recombination of genes, an enormous diversity of TCRs. TCR expression is followed by selection:
- Positive selection - interaction of immature thymocytes with low TCR expression with the major histocompatibility complex (MHC, the genetic system responsible for distinguishing self from foreign - mainly the HLA complex, Human Leucocyte Antigen) on the epithelium (CD4 - HLA II, CD8 - HLA I) → cell selection capable of interacting with a foreign antigen (Ag) presented by its own MHC.
- Negative selection – thymocytes with high expression of TCR reacting with self-peptides presented with HLA I or II on thymic macrophages → induction of apoptosis → deletion of autoreactive clones.
T-cells then migrate to the secondary lymphatic organs.[3]
B-cell development[edit | edit source]
The development of B-cells takes place in several stages:
- phase without the presence of Ag (antigen-independent development):
- They develope from progenitor cells in the bone marrow: HLA-DR+, CD45+, CD34+, CD19+.
- They require contact with the bone marrow stromal cells (VCAM-1 + early lymphocyte VLA-4), cytokine SCF (Stem Cell Factor) and IL-7.
- Naive (virgin) mature B-cells have IgM, IgD on their surface.
- In the bone marrow, there is a negative selection of autoreactive B-cell clones (those which strongly react with their own Ag) - induction of apoptosis, induction of rearrangement of gene segments for the BCR, blocking and anergy.
- phase with Ag stimulation (antigen-dependent development):
- Occurs in the secondary lymphoid organs (nodes, spleen, mucousa), B-cells get into contact with T-cells and antigen-presenting cells.
- It takes place in 2 phases – the primary and secondary phase of the antibody response:
- Primary phase of the antibody response (primary response)
- It takes place in primary lymphoid follicles (in nodes) where B-cells interact with Ag on APC and with Th2.
- When a naive mature B-cell comes into contact with an antigen (Ag), the following occurs:
- Recognition of the antigen (Ag) through antigen-specific receptors on B-cells (BCR = B-cell receptor);
- B-cell stimulation by BCR + Ag binding;
- Ag uptake → Ag presentation on HLA II. precursors of Th-cells→ formation of antigen-specific Th2.
- B-cell = APC for T-lymphocyte.
- The contact of T-cells and B-cells is enabled via CD28 + CD80/86, CD40L + CD40 and leads to the multiplication of B-cells and differentiation into:
- Secondary phase of the antibody response (secondary response)
- After repeated exposure of the memory B-cell to the antigen, the production of a larger number of cells occurs and is accompanied by:
- Affinity maturation = change of the BCR;
- Formation of secondary lymphatic follicles with a germinal center;
- Antibody class switching - IgG, IgA, IgE;
- The formation of plasma and memory cells with a higher affinity to Ag (somatic mutations of Ig genes increase the affinity of antibodies).
- Secondary response result = Ig with higher affinity to Ag able to activate complement and opsonize (IgG+FcR). [3]
Primary and secondary responses to each other during typical infections immediately follow and lead to the formation of memory cells. In case of repeated infection (subsequent encounter with Ag):
- The level of Ig persists - immediate suppression of infection.
- Memory cells are rapidly activated to produce high-affinity Ig of different isotypes . [5]
- Terminal maturation into plasma cells :
- Differentiation to memory cells (for a certain Ag) and plasma cells (secretion of Ag-specific Ig = antibodies).
- Ig isotypes: G, A, M, E, D.[3]
Postnatal lymphopoiesis[edit | edit source]
T-cells[edit | edit source]
The umbilical cord blood has a higher number of T-cells (CD3+) than the blood in infants. The CD4:CD8 ratio is higher. T-lymphocytes have the ability to respond to a mitogenic stimulus and induce an antigen-specific response (see e.g. BCG vaccine).
B-lymphocytes[edit | edit source]
There is a higher number of B-lymphocytes in the umbilical cord blood. However, they do not yet form the entire spectrum of immunoglobulins (Ig). After stimulation by antigens (Ag) from the external environment, IgM is first formed (this ability is also present in immature B-lymphocytes). The total Ig level is lowest around 3 to 4 months of age. The ability to form Ig against protein Ag is present from birth, but the ability to form Ig against polysaccharide Ag is non-efficient until 2 years of age (polysaccharide vaccine is not suitable, rather a conjugate vaccine must be used, e.g. against Haemophilus influenzae type B). The newborn is more susceptible to G- infection because the lack of IgM (= opsonins ) causes imperfect phagocytosis of polymorphonuclears. The maternal IgGs work as opsonins for most G+ bacteria, specific IgGs are sufficient against common virus infections. Premature infants have less maternal IgG and therefore lower opsonization activity for all types of microorganisms.[3]
Lymphatic organs development[edit | edit source]
- Thymus – at birth, it has 2/3 of the adult weight, it is largest just before puberty, after which there occurs a gradual involution.
- Peripheral lymphatic tissues - adult size up to 6 years of age, larger in prepubertal period, then involution.
- Spleen - gradually grows into adulthood.
- Peyer's patches - grow gradually, are largest during adolescence. [3]
Links[edit | edit source]
Related articles[edit | edit source]
- Primary immunodeficiency
- Defects in cellular immunity
- Defects of humoral immunity
- Severe combined immunodeficiency
References[edit | edit source]
- ↑ LEBL, J – JANDA, J – POHUNEK, P. Klinická pediatrie. 1. edition. Galén, 2012. 698 pp. pp. 223. ISBN 978-80-7262-772-1.
- ↑ http://fvl.vfu.cz/export/sekce_ustavy/mikrobiologie/imunologie/Prednasky/02_8_bunky_organy_bariery.pdf
- ↑ Jump up to: a b c d e f http://www.vfn.cz/pracoviste/kliniky-a-oddeleni/klinika-detskeho-a-dorostoveho-lekarstvi/
- ↑ http://jeeves.mmg.uci.edu/immunology/CoreNotes/Chap17.pdf
- ↑ Jump up to: a b eamos.pf.jcu.cz/amos/kpk/externi/kpk_2816/8.ppt