Bradyarrhythmia
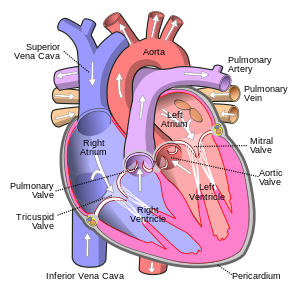
Bradycardic disorders are caused either by a disorder in the sinus node or by a blockage of the conduction of excitement from the atria to the ventricles. The most common is sinus bradycardia.
Sinus bradycardia[edit | edit source]
This is a slowing of the heart rate <60 / min. Physiologically, it occurs in situations where vagal activity predominates (sleep). Normally, this kind of value can be found in athletes, in which it reaches 40 beats per minute. Possible causes include for example: hypothyroidism, hypothermia, intracranial hypertension, Myocardial Infarction of the lower wall, sick sinus syndrom. It is also often induced iatrogenically by Beta-blockers, verapamil, digitalis or amiodaron.
Therapy - in symptomatic individuals atropine 0.5-1 mg iv
Sick sinus syndrome[edit | edit source]
It is a permanent or paroxysmal sinus bradycardia, until the sinus arrest. It can be alternated with flutter / atrial fibrillation . Excitement disorder occurs, which may be functional / anatomical and transient / permanent.
Ethiology[edit | edit source]
- Idiopathic degenerative damage in the area of the SA node
- Ischemic heart disease,
- cardiomyopathy,
- increased vagotonia,
- endocrinopathy ,
- medications
- direct damage to the sinus node.
The clinical picture[edit | edit source]
Most patients are asymptomatic. Otherwise they experience palpitations, dizziness, confusion, pre-syncopies, syncope and they can also suffer from a lower minute cardiac output.
Diagnosis[edit | edit source]
On the ECG we observe a slow or irregular sinus action, various surrogate rhythms or, conversely, paroxysms of tachycardia.The negative effect of the autonomic nervous system confirms the ability of the sinus node to increase heart frequency during exercise (confirmed by ergometry). Holter ECG shows the variability of heart frequency during the day and night, episodes of sinus pauses or the occurrence of other severe arrhythmias.
Therapy[edit | edit source]
Asymptomatic patients do not require treatment. In bradycardia with a hemodynamic disorder, we indicate a pacemaker implantation.
Sinus arrest[edit | edit source]
This is an outage of various lengths in the SA node. With a longer pause, junctional or idioventricular contraction may occur. It may be clinically manifested bt syncope.
Therapy - in symptomatic individuals atropine 0.5-1 mg iv
Sinoatrial blockade[edit | edit source]
It has three degrees, but only the III. degreeis clinically significant. In this case, a pulse is not transferred from the sinus node to the atrial myocardium → loss of a single heartbeat. The entire P-QRS-T complex is missing from the ECG.
Therapy - in symptomatic individuals atropine 0.5-1 mg i.v. [1]
Atrioventricular block[edit | edit source]
This is a disorder in the transfer of the depolarization wave to the ventricules. Blockade is most often in the AV node (suprahisally), but can also occur in the His bundle (intrahisally) or infrahisally.
AV-Blocks:
Etiology[edit | edit source]
- Myocardial Infarction (especially of the lower wall with closure of the coronary artery),
- inflammation - viral myokarditis, borreliosis, Changeas disease
- trauma,
- bradycardizing drugs - digoxin , beta-blockers,
- idiopathic fibrosis,
- cardiomyopathy.
Degrees[edit | edit source]
1st degree[edit | edit source]
Prolonged AV conduction of excitement, therefore PQ> 0.2 s. Carditis in acute rheumatic fever , digoxin intoxication, β blockers. Clinically insignificant, it must be taken into account when medicating with the above drugs.
2nd degree[edit | edit source]
Intermittent outages from the atrium to the ventricles (some excitations do not pass to the ventricles), P waves not followed by the QRS complex occur on the ECG.
AV block II, Mobitz type I (Wenckebach)[edit | edit source]
With each excitation transmitted, the disorder escalates and the conduction time of the excitation from the atria to the ventricles increases. Eventually, the conduction failure escalates so that the excitement from the atria to the ventricles is not transferred. A temporary complete blockage of the AV transfer occurs. Failure to convert the excitement will allow the transmission system to "recover" and resume the AV transmission. This process repeats periodically. The interval from one complete AV block to another complete AV block is called the Wenckebach period.
The more severe the disorder, the sooner a complete AV block will occur and the shorter the Wenckebach period. The usual ratio of AV conversion is 5: 4, 4: 3 and 3: 2. In the last case, the Wenckebach period can be shortened so that a complete AV block occurs after each successful AV conversion. The transfer system can handle one excitation transmission from the atrium to the ventricles, but can no longer handle another AV transmission. This disorder is called the fixed Wenckebach period . There is an AV conversion ratio of 2: 1 (every second P wave is converted).
The fixed Wenckebach period , unlike Mobitz II AV block , is not a clear indication for pacemaker implantation. The exception is symptomatic bradycardia in a fixed Wenckebach period. For example, if the patient's SA node frequency drops to 60 / min, then with AV conversion 2: 1, the QRS and ventricular systolic frequency will be 30 / min, and this will usually cause a significant decrease in cardiac output. If the SA node function is OK, the sympathetic system resolves the 2: 1 AV block by stimulating the SA node to a higher node rate, such as 120 / min to maintain a QRS (ventricular systole) rate of 60 / min.
ECG findings[edit | edit source]
On the ECG, there is a P wave in front of each QRS complex , the rhythm is sinusoidal and the QRS complex lasts a maximum of 0.12 s . With each new P-QRS complex, the PQ interval gradually lengthens as the AV transmission failure progresses . When a complete AV block occurs, a P wave (evidence of atrial depolarization) is displayed on the ECG, which is not followed by a QRS complex (evidence of a complete AV block). After a pause, a P-QRS complex appears on the ECG , usually with a normal PQ interval (evidence of renewed AV conduction).
Localization of lesions[edit | edit source]
The lesion in the transmission system is located predominantly in the AV node, less often in the His bundle . The location of the disorder cannot be determined from the surface ECG, but only by invasive electrophysiological examination.
AV block II, Mobitz type II.[edit | edit source]
At normal heart rate, the damaged area fails to transfer all control pulses from the AV node to the ventricles. Each converted pulse induces a complete blockage of the AV transmission (both Tawara branches do not conduct). Místo poruchy potřebuje určitou dobu na zotavení k tomu, aby mohlo dojít k dalšímu A-V převodu.The fault location needs some recovery time for further AV conversion to occur. At the mildest degree of disturbance, the control pulses from the supraventricular region are converted to chambers in a 2: 1 ratio (PP-QRS). At a higher degree of failure, the AV conversion ratio increases to 3: 1, 4: 1, etc. As the Tawar arm progresses, it completely stops the excitement and a complete III ° AV block occurs (there is a conduction block in both Tawar arms).
This type of AV block is unstable and usually progresses to a complete III ° AV block with ventricular bradycardia, or worse, asystole and syncope (Adams-Stokes syndrome). Therefore, the finding of Mobitz II on the ECG is very important and is an indication for the patient to be placed on a monitored bed and for early implantation of a pacemaker. For the above reasons, the name Mobitz II should not be used for AV block with a 2: 1 ratio and QRS complex shorter than 0.12 s. , verapamil or diltiazem, digoxin), hyperkalaemia and hypothyroidism. About 20% of patients with 2: 1 AV block have an intermittent His-bundle lesion and a pre-existing permanent conduction block in one of the Tawar arms (PP-QRS ...; and QRS wider than 0.12 s). In terms of lesion location, it is a fixed Wenkebach period with AV transmission 2: 1 and this disorder usually does not have the risk of significant bradycardia as AV block Mobitz II °. However, these disorders cannot be distinguished from normal ECG recording. In both cases, the QRS complex will be wider than 0.12 s, each QRS complex will be preceded by 2 P waves and the PQ interval will be constant.
ECG findings[edit | edit source]
There is a larger number of P waves per QRS complex on the ECG (PP-QRS… PPP-QRS… PPPP-QRS). The PQ interval is constant (ventricles are controlled from the supraventricular area and if it is the SA node the sinus rhythm remains. QRS is wider than 0.12 s (there is a ventricular conduction defect - blockage of the Tawara branch).
Localization of lesions[edit | edit source]
In 80% of these disorders, the lesion in the transmission system is located in one of the Tawara branches . The lesion is distal to the bifurcation of His's bundle in a situation where the second Tawara branch does not conduct at all (at the same time a complete blockage of conduction in the contralateral Tawara branch).
3rd degree[edit | edit source]
Permanent complete AV block. None of the supraventricular excitations reach the ventricules.
It occurs either as progression of a Mobitz II ° blockade or by sudden damage to the conduction system, for example in acute myocardial infarction.
AV block III ° with ventricular rhythm is a clear indication for pacemaker implantation. Implantation is postponed in reversible causes of AV conduction block (acute diaphragmatic myocardial infarction, bradycardic drugs, hyperkalemia, hypothyroidism, infectious endocarditis). In contrast, pacemaker implantation is not postponed in the onset of III ° AV block in acute anteroseptic myocardial infarction. Severe bradycardia usually does not occur in III ° AV blocks with a QRS complex shorter than 0.12 s (40% of AV blocks) (the alternative ventricular control center is supraventricular). If the surrogate center has a frequency greater than 40 rpm, this complete AV block is not an indication for pacemaker implantation.
ECG findings[edit | edit source]
P waves appear on the ECG independently of QRS complexes wider than 0.12 s (there is a junctional or idioventricular rhythm, usually SF <40 / min). There is AV dissociation in which P waves have a higher frequency than QRS complexes.
Localization of lesions[edit | edit source]
In 61% of all III ° AV blocks, the lesion is located in one of the Tawara branch with the current previous conduction block in the contralateral Tawara branch..
Therapy[edit | edit source]
1st degree[edit | edit source]
- not treated.
2nd degree[edit | edit source]
- elimination of potential cause - antiarrhythmic treatment, digoxin, hyperkalemia, myocardial ischemia, hypotension
- type I:
- atropine: 0.02 mg / kg iv, io, et, i.e. 0.1 mg / 5 kg (0.2 ml) in symptomatic individuals;
- type II:
- alternatively isoprenaline 0.02 mg / kg;
- implantation of a permanent pacemaker
- temporary cardiostimulation in symptomatic and asymptomatic acute myocardial infarction
3rd degree[edit | edit source]
- elimination of potential cause - antiarrhythmic treatment, digoxin, hyperkalemia, myocardial ischemia, hypotension
- atropine or temporary cardiostimulation
- continuous cardiostimulation in chronic symptomatic AV block with heart failure.
Principles of pacemaker implantation[edit | edit source]
| Cardiostimulators | |||
|---|---|---|---|
| Diagnosis | Stimulation mode | ||
| Optimál | Possible | Inappropriate | |
| Sick sinus syndrome | DDD(R) | AAI(R) | VVI, VDD |
| AV blockade | DDD | DD | AAI, DDI, VVI + VA conduction |
| SSS + AV block or branch block | DDDR, DDIR | DDD, DDI | AAI, VVI |
| Permanent atrial fibrillation or atypical atrial flutter | VVI(R) | VVI | AAI, DDD |
| SSS or AV block + paroxysmal atrial arrhythmias | DDDR + AMS | DDIR, DDDRP + AMS | VDD, AAI |
| Heart Failure | DDD BiV | VVIR BiV | AAI, VDD |
| Hypertrophic cardiomyopathy | DDD + optimalized AV delay | VDD, DDDR + optimalized AV delay | AAI, VVI |
| BiV: biventricular stimulation, DDDRP: dual-cavity rate-responsive pacing using preventive atrial pacing algorithms in patients with paroxysmal atrial fibrillation | |||
| taken from [2] | |||
Links[edit | edit source]
External links[edit | edit source]
- Sinus bradycardia and ECG - Free ECG book
- [1]
Source[edit | edit source]
- HAVRÁNEK, Jiří: Arytmie.
- PASTOR, J. Langenbeck's medical web page [online]. [cit. 2009]. <https://www.freewebs.com/langenbeck/>.
- WEBERNDÖRFER, Vanessa – RUSSI, Ian – KOBZA, Richard. Cardiovascular medicine [online]. ©2018. [cit. 2022]. <https://cardiovascmed.ch/article/doi/cvm.2018.00580>.