Brenner tumor
Brenner tumor (Brenner carcinoma, ICD-O: 9000/0 is a mixed ovarian fibroepithelial tumor. It is a relatively rare tumor, it represents about 2% of all ovarian tumors, 71% of cases are demonstrated in people over the age of 40. It is mostly a benign tumor, but borderline and malignant variants can also occur. Although it is an ovarian tumor, it can rarely occur in other locations, especially in other areas of the female genital tract. The Brenner tumor itself can rarely be the target of the metastatic process
The actual histogenetic origin of Brenner's tumor is not a closed question, most authors assume that the tumor originates from the surface epithelium of the ovaries, which metaplastically changes into urothelium.
Benign Brenner tumor[edit | edit source]
ICD-O: 9000/0
Benign Brenner tumor is the most common variant of Brenner tumor. It represents 4 to 5% of benign ovarian tumors, usually diagnosed in women between 30 and 60.
Macroscopic appearance[edit | edit source]
Macroscopically, Brenner's tumor is relatively dense, solid, and similar to fibroma. It tends to have well-defined border and the usual size at diagnosis is 2 cm, only 10% of cases are over 10 cm in diameter. In section, the structure is relatively fine-grained, white to yellow in color. Deposits of calcification may be present, and the presence of cysts is quite common. Association with another tumor, especially mucinous cystadenoma, is not rare.
Histological appearance[edit | edit source]
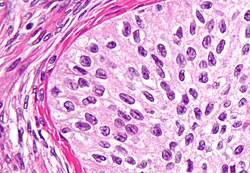
The epithelial component is represented by not quite regular nests or stripes of light, sharply demarcated polygonal cells characteristic of urothelium (transitional epithelium). The nucleus of these cells has a central groove that gives it the appearance of a coffee bean character. Cytoplasm is abundant, bright. Nests may have a central cavity in which eosinophilic material then accumulates, staining with mucin. In addition to the morphological ones, the epithelial component shows some immunochemical characteristics similar to the urothelium (urothelin expression), but others are absent (thrombomodulin expression) or have only been demonstrated inconsistently (cytokeratin 20 expression).
The stroma is relatively cellular, clearly mesenchymal character. It sharply borders individual nests of epithelial cells. The stroma can undergo luteinization and then it is very likely capable of producing sex hormones.
Clinical behavior[edit | edit source]
Most benign Brenner tumors are asymptomatic, only greatly enlarged tumors may present nonspecifically as a mass in the small pelvis. The stromal component can sometimes undergo focal luteinization, and the tumor can then manifest itself as an overproduction of sex hormones. Ascites appears only rarely.
Border-line Brenner tumor[edit | edit source]
ICD-O: 9000/1
A border-line tumor already shows atypia in the epithelial component compared to a benign tumor, but there is no demonstrable stromal invasion. It represents about 3 to 5% of all diagnosed Brenner tumors.
Macroscopic appearance[edit | edit source]
A border-line is usually quite large at the time of diagnosis, typically measuring 16–20 cm in diameter. It usually contains components similar to a benign Brenner tumor and foci of a cystic component in which papillary or polypoid masses may be present. Bilateral occurrence is rare.
Histological appearance[edit | edit source]
The structure of the tumor is richer, the fibrovascular stroma can lead to the rise of a papillary structure. The mitotic activity of the epithelial component is variable but may be substantial. Focal necrosis and mucinous metaplasia, which can sometimes dominate the entire picture, are relatively common.
Clinical behavior[edit | edit source]
The tumor presents clinically as masses in the small pelvis or abdominal pain, sometimes it can be the cause of abnormal vaginal bleeding. Not a single case of metastatic spread or even death has been described in a patient with Brenner tumor, without stromal invasion, only local recurrence is at risk.
Malignant Brenner tumor[edit | edit source]
ICD-O: 9000/3
In the case of a malignant Brenner tumor, the epithelial component behaves malignantly. The tumor usually also contains foci of benign Brenner's tumor. The malignant variant accounts for about 5% of all Brenner tumors. It occurs most often in women between the ages of 50 and 70.
Macroscopic appearance[edit | edit source]
In appearance, a malignant Brenner tumor is similar to a border-line tumor. It is usually 16–20 cm in diameter at the time of diagnosis, and contains both a solid component and cystic formations on section. Tumor masses in the form of papillary to polypous formations can grow into cysts. Bilateral involvement occurs in 12% of cases.
Histological appearance[edit | edit source]
The histological picture usually shows a benign or border-line tumor in which a component invading the stroma is present. The invasive components are usually of the nature of a high-grade transitional cell tumor or squamous cell carcinoma. Glandular and mucinous structures may also be present. Foci of calcification are often present, in some cases calcification can dominate the histological picture. Sometimes the mucinous metaplasia can be so pronounced that the structures of the Brenner's tumor are barely visible and can easily be missed.
Clinical behavior[edit | edit source]
Clinical manifestations tends to be the same as for a border-line tumor, i.e. manifestations of the presence of a tumor mass in the small pelvis, abdominal pain and sometimes abnormal vaginal bleeding.
80% of malignant Brenner tumors are caught at stage I. Five-year survival of patients at stage IA is 88%.
Links[edit | edit source]
Literature[edit | edit source]
- MOTLÍK, Karel – ŽIVNÝ, Jaroslav. Patologie v ženském lékařství. 1. edition. Praha : Grada Publishing, 2001. ISBN 80-7169-460-6.
- TAVASSOLI, Fattaneh A. – DEVILEE, Peter. WHO Classification of Tumours : Pathology and Genetics of Tumours of the Breasts and Female Genital Organs [online] . 1. edition. Lyon : IARC Press, 2003. Available from <http://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb4/index.php>. ISBN 92-832-2412-4.
- ROSAI, Juan. Ackerman's Surgical Pathology. 8. edition. St. Louis, MO. 1996. 2; ISBN 0-8016-7004-7.
External links[edit | edit source]
- Brenner tumors - general on the website PathologyOutlines.com
- Benign Brenner tumor on the website PathologyOutlines.com
- Borderline Brenner tumor on the website PathologyOutlines.com
- Malignat Brenner tumor on the website PathologyOutlines.com