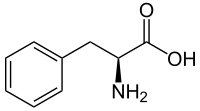
Congenital disorders of phenylalanine metabolism
This is a group of autosomal recessive hereditary diseases in which hyperphenylalaninemia occurs in the body. The gene is located on the 12th chromosome, the incidence is 1:10,000.
We distinguish 2 forms:
- classic phenylketonuria (PKU) - a defect in the enzyme phenylalanine hydroxylase;
- atypical phenylketonuria - defect or disorder of dihydrobiopterine reductase biosynthesis.
A phenylalanine level higher than 0.6 mmol/l is called hyperphenylalaninemia.
In PKU, there is insufficient conversion to tyrosine due to a malfunction of the aforementioned enzyme. The disease has long been part of newborn screening. Clinical symptoms in untreated children include: arrest of psychomotor development in infancy to toddlerhood, drug-resistant epilepsy, and skin hypo-pigmentation. The baby's urine tends to smell like mouse droppings. Diet therapy is lifelong and is based on the administration of a diet with reduced phenylalanine content. In some patients, the effect of sapropterine dihydrochloride, which reduces the level of phenylalanine, is good.
Pathogenesis[edit | edit source]
Phenylalanine and its alternative metabolites (phenylpyruvic, phenyllactic, phenylacetic and o-hydroxyphenylacetic acid) accumulate in the body and are excreted in the urine. Dysbalance of plasma AMK damages the development of the brain, up to 6 years of age of the child. Furthermore, enteral resorption of tyrosine, which uses the same transporter as phenylalanine, is inhibited. Since tyrosine is also involved in the production of the melanin pigment, its synthesis is disrupted and therefore the pigmentation of the skin and hair is reduced.
Newborn Screening[edit | edit source]
For newborn screening, we use capillary blood from the 2nd-3rd leg one day after birth. At the time of collection, the newborn should be on milk formula. If the newborn was discharged between the 2nd and 3rd day, we will perform the test, but after discharge the practitioner will arrange for capillary blood to be collected for follow-up examination. Today we use the method of tandem mass spectrometry.
Diagnostic[edit | edit source]
The basis is the already mentioned blood sampling, which will be used for metabolic and molecular diagnostics. Liver biopsy enzyme testing is not required for diagnosis or treatment, but all children with PKU should be tested for pterin metabolism to differentiate the forms.
Clinical picture without treatment[edit | edit source]
Shortly after birth, the child has no clinical symptoms but he gradually lags behind in psychomotor development. He often vomits, is hyperactive and makes aimless movements of the nature of athetosis. Epileptoform convulsions and EEG changes are also common.
At the same time, we can observe: microcephaly, light hair on the body of the child, blue eyes and changes in the nature of seborrheic dermatitis or eczema on the pale skin. The sweat smells strongly of mouse droppings.
Therapy[edit | edit source]
The basis is a low-phenylalanine diet, which is lifelong. It is a type of nutrition with a reduced intake of phenylalanine. This can be achieved by selecting foods with low levels of phenylalanine and using food supplements without phenylalanine. The daily need for AMK must be supplemented with a mixture of essential AMK without phenylalanine, enriched with ions, trace elements, vitamins and especially tyrosine (due to the fact that the body is not able to create it endogenously, or only in a minimally insufficient amount, so for phenylketonurics it is essential). We always consider the age of the child. The diet must be strictly followed during pregnancy, where there would be a risk of psychomotor retardation of the fetus, microcephaly or the development of VSV.
The target value of phenylalanine is 100−300 µmol/l.
Another option is enzyme therapy using the pegvaliase enzyme. This is administered subcutaneously and converts phenylalanine in the bloodstream to ammonia and trans-cinnamic acid. The disadvantage of this therapy is its financial burden and its immune reaction to the enzyme molecules. The main advantage is that patients tolerate higher levels of phenylalanine better and can moderate their diet as a result.
Links[edit | edit source]
Related articles[edit | edit source]
External resources[edit | edit source]
Source[edit | edit source]
- BENEŠ, Jiří. Studijní materiály [online]. ©2007. [cit. 2010-04]. <http://www.jirben.wz.cz/>.
References[edit | edit source]
- HRODEK, Otto a Jan VAVŘINEC, et al. Pediatrie. 1. vydání. Praha : Galén, 2002. ISBN 80-7262-178-5.
- ŠAŠINKA, Miroslav, Tibor ŠAGÁT a László KOVÁCS, et al. Pediatria. 2. vydání. Bratislava : Herba, 2007. ISBN 978-80-89171-49-1.
- LEBL, Jan, Jan JANDA a Petr POHUNEK. Klinická pediatrie. 2. vydání. Galén, 2012. 698 s. ISBN 9788072627721.