Diabetes mellitus
Diabetes mellitus (DM) is a chronic metabolic disease with high morbidity and mortality, with the major manifestation of hyperglycemia due to absolute or relative insulin insufficiency. In the last decade, there has been a significant and steady increase in the incidence of diabetes mellitus worldwide, including in Czechia. Especially in economically developed countries, the cause of this phenomenon lies in the population's lifestyle, such as excessive energy intake and reduced physical activity.
At present, more than 10% of the population are diagnosed with diabetes mellitus in Czechia (approximately 990,000 individuals). Estimates suggest that at least 5% more of the population with diabetes mellitus remains undiagnosed. These are most often type 2 DM (93% of cases), type 1 DM makes up about 5%, and other types are less common.
Classification of diabetes mellitus[edit | edit source]
- Diabetes mellitus type 1
- Autoimmune
- Absolute lack of insulin production by the pancreatic beta cells of Islet of Langerhans
- Usually affecting the younger population
- Requires administration of insulin
- Diabetes mellitus type 2
- Resistance to the action of insulin
- Usually affecting adults and the older population
- The production of insulin could even be increased in the earlier course of the disease, with reduction in the later course of the disease
- Weight management, diet control, and exercising are essential, if still insufficient, diabetic medications or insulin therapy might be required
- Gestational diabetes mellitus
- DM that occurs during pregnancy, which resolves soon after delivery
- Pregnant women should undergo a 2-phase screening:
- Phase I: In the first trimester of pregnancy (up to the 14th week), assessment of fasting blood glucose
- Phase II: Women who test negative for Phase I are subjected to Phase II of screening. The oral glucose tolerance test (oGTT) is evaluated.
- Women who experience gestational DM have an increased risk of developing DM type 2 later on in life
- Other specific types of diabetes mellitus
- DM in endocrinopathies (acromegaly, pheochromocytoma, hypercortisolism, hyperthyroidism, etc.)
- Drug and chemical-induced DM (glucocorticoids, nicotinic acid, thyroid hormones)
Pathogenesis[edit | edit source]
Disruption of glucose metabolism occurs with:
- Impaired insulin production or secretion (insulin deficiency
- Impaired response to insulin (insulin resistance)
- Possibly a combination of both mechanisms
Insufficient insulin function disrupts the transport of glucose from the blood to the cell, leading to hyperglycemia and glucose deficiency intracellularly. Insufficient glucose utilization leads to a change in the mechanisms for ATP gain. Gluconeogenesis and glycolysis are stimulated, while lipolytic breakdown of triacylglycerols into fatty acids and glycerol increases in adipocytes. Degradation of fatty acids by β-oxidation produces excess acetyl-CoA, from which ketones (acetoacetate, 3-hydroxybutyrate, and acetone) are formed in the liver. Acetacetate can serve as a source of energy for muscle and brain activity instead of glucose.
If the production of ketone bodies exceeds their utilization by peripheral tissues, ketoacidosis develops (with characteristic clinical sign of fruity breath). Because ketone bodies are soluble in water and excreted in the urine, ketonuria could occur as well. When the plasma glucose concentration threshold (10-12 mmol/L) is exceeded, the transport capacity of the proximal tubule is disrupted and glucose is excreted into the final urine. As glucose and ketone bodies are osmotically active, this leads to osmotic diuresis, which causes additional water to be loss in urine bringing about polyuria.
Clinical aspects[edit | edit source]
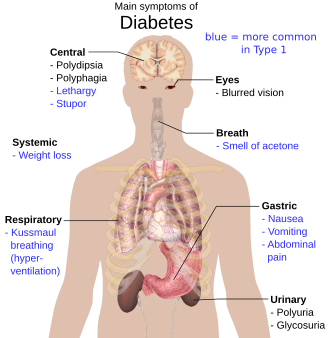
The characteristic signs include:
- DM type 1: thirst, polydipsia, polyuria, weight loss
- DM type 2: is often associated with obesity
Psychological aspects of treatment[edit | edit source]
Due to the need for comprehensive treatment of the disease, cooperation at the doctor-patient level is important. A patient with DM may experience problems such as those associated with the necessary precautions (e.g. restrictive diet) or related secondary complications that may lead to diabetic distress. It is appropriate for the doctor to focus on the psychological aspects of this disease as well.
Complications[edit | edit source]
- Acute complications
- Hypoglycemia,
- Diabetic hyperosmolar hyperglycemic coma,
- Diabetic ketoacidosis
- Ketoacidotic coma
- Lactic acidosis,
- Lactacidotic coma.
- Chronic complications
- Diabetic kidney disease
- Diabetic retinopathy,
- Diabetic neuropathy,
- Diabetic foot syndrome
- Atherosclerosis
History of the treatment of DM[edit | edit source]
One of the most important events in the history of diabetes treatment was in the year 1921, when Frederick Grant Banting and his assistant, medical student Charles Herbert Best, discovered a substance in the animal pancreas that caused the dogs' plasma glycemia levels to drop. This substance was named 'insulin'. The experiment was later repeated on a 13-year-old boy suffering from DM type 1, Leonard Thompson, who became the first person to be injected with insulin.
References[edit | edit source]
Sources[edit | edit source]
- ČEŠKA, Richard, et al. Interna. 3. vydání. Praha : Triton, 2020. 970 s. ISBN 978-80-7553-780-5.