Ectopic pregnancy
Ectopic pregnancy (GEU - graviditas extrauterina) is defined as the implantation of a blastocyst outside the uterine cavity. It is the most common cause of sudden abdominal episode in gynecology. The incidence is about 2 per 100 pregnancies and has an increasing trend due to more frequent cases of IVF. The most common location is the ampullary region of the fallopian tube (more than 80%).
Etiopathogenesis[edit | edit source]
The causes of ectopic pregnancy can be post-inflammatory (after salpingitis, after surgery on the fallopian tubes). Other reasons are hormonal imbalance (disorder of fallopian tube motility), smoking, endometriosis, fallopian tube torsion, adhesions in the abdominal cavity, scar after cesarean section. GEU is often found in women who have undergone ovarian stimulation, in vitro fertilization, or use of IUD, etc..
Intrauterine and extrauterine pregnancies can coexist as so-called heterotopic pregnancies with a high risk of overlooking just the ectopic component. It is particularly risky in women who have undergone IVF or medical treatment for sterility.
Clinical picture[edit | edit source]
The death of the embryo in GEU usually occurs between the 6th and 10th gestational week due to unfavourable nidation conditions. The clinical picture depends on the localization and may be asymptomatic. In general, the classic subjective symptoms of early pregnancy are present, although usually less pronounced than in normal pregnancy (morning sickness, vomiting, breast tightness).
- Pain
- Lower abdominal pain is a key symptom and should always raise suspicion of GEU in women of childbearing age. They manifest most commonly between the 6th and 8th week of gestation, i.e. a short interval from delayed menstruation. They are tensive and variable pains that may be accompanied by peritoneal irritation (e.g. blood leakage into the abdominal cavity). In the case of tubal localization of GEU, the pain increases over time.
- Bleeding
- A typical sign is so-called spotting, that is, small blood losses. A possible symptom is recurrent or prolonged bleeding. Only amenorrhoea may be present.
- Symptoms accompanying some complications
- Abortus tubarius is accompanied by intense and sudden spasmodic pains of a colicky character corresponding to contractions of the musculature of the fallopian tube in the attempt to expel the abortion into the uterus. The patient may then become completely asymptomatic, but the pain may return under the picture of peritoneal irritation caused by bleeding into the abdominal cavity. However, it is less intense than in the case of fallopian tube rupture.
- Rupture of the tube is a sudden abdominal episode arising precipitously in a perfectly healthy patient. It has a fulminant course leading to a state of shock.
Localization[edit | edit source]
- Tubal pregnancy
- It affects 85-90% of the ampullary part, 10-15% of the isthmus and rarely also the pars uterina. Two complications may occur. The first complication is abortus tubarius (typically when GEU is located in the ampulla) with expulsion of the embryo either retrograde into the peritoneal cavity or rarely into the uterus, all due to contractility of the fallopian tube wall.
- The second complication may be rupture of the fallopian tube wall, which occurs most often when the GEU is deposited in the isthmus or pars uterina, which are the narrowest parts of the fallopian tube and as such have very limited distensibility. This can easily lead to perforation and subsequent wall rupture with potentially lethal bleeding into the abdominal cavity.
- Ovarian pregnancy
- Very rare. The situation occurs if the egg is not released from the ruptured follicle and fertilization of the sperm occurs already at the level of the ovary.
- Peritoneal/abdominal pregnancy
- They represent 1% of the total number of GEUs. Most often it occurs in secondary implantation due to tubal abortion or uterine tube rupture. Bleeding complications are particularly common when the placenta is implanted on a highly vascularized organ, especially in the epigastrium. Abdominal localizations are rare and often late recognized because of the minimal accompanying symptoms they induce. Clues to the correct diagnosis may be persistent, diffuse abdominal pain and nausea that does not resolve even in the relatively late stages of pregnancy.
- Other forms
- Intramural (in the myometrium) is a rare form occurring in female IUD carriers. Cervical occurs as a consequence of disturbed decidual transformation of the endometrium or delayed blastocyst maturation. Incompatible with fetal life and threatening to the mother if the placenta causes erosion of the arteria uterina.
Diagnostics[edit | edit source]
An ectopic pregnancy is usually diagnosed either as part of normal pregnancy checks or as an acute condition when one of the complications arises. The diagnosis is based on the following procedures.
- Anamnesis
- Risk factors need to be addressed.
- Physical examination
- Speculum examination reveals typical dark brown traces of bleeding. With peritoneal irritation, this examination may cause unusually severe pain described as knife-like. Tactile bimanual examination must be performed with caution as rupture of the fallopian tube could occur. Palpation of the abdomen will reveal intense unilateral pain or diffuse tenderness. However, both may be absent.
- Laboratory examination
- The most important for diagnosis are serum beta-hCG levels, which confirm an ongoing pregnancy. The addition of ultrasound will detect ectopic localization of the embryo or its absence in the uterine body.
- Ultrasound
- We always perform abdominal and vaginal ultrasound examinations. The purpose is to rule out or confirm extrauterine pregnancy, assess other complications in the abdominal cavity and the presence of free fluid in the small pelvis and Douglas space.
More detailed information can be found on the page Diagnostic imaging methods in gynaecology.
- Overall status
- It is necessary to pay special attention to the onset of symptoms of hypovolemic shock (tachycardia, hypotension, etc.). Fever is not a direct indicator; it may be a reaction to resorption, as in the case of intra-abdominal haemorrhage, or a secondary infection.
Differential diagnosis[edit | edit source]
From the beginning of the patient's acute admission to the time of receipt of the pregnancy test results, the differential diagnosis is quite extensive. Considerations include salpingitis, intrauterine abortion, ovarian or tubal torsion, ruptured ovarian cyst, myoma necrosis, pyelonephritis, appendicitis, cystitis, renal lithiasis.
Treatment[edit | edit source]
The goal is primarily to end GEU due to the potentially fatal complications threatening the mother. Medical and surgical therapies may be considered.
Systemic treatment with methotrexate[edit | edit source]
Methotrexate is a cytostatic that blocks DNA synthesis in rapidly growing tissues. Its use requires meeting strict criteria and is therefore only applicable in 1/3 of patients. It is reserved for early diagnosed GEU of all localizations. If the conditions of application are optimal, the success rate of the method is up to 95%. However, it is not widely used in our country due to numerous side effects.
Surgical solution[edit | edit source]
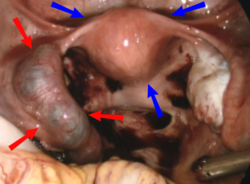
Except in acute situations with haemodynamic instability, when laparotomy is indicated, laparoscopy is the method of choice in most cases. Given the most common localization of GEU within the uterine tube, the standard operative treatment for tubal pregnancy is salpingectomy and salpingotomy.
- Salpingectomy
- Thus, removal of the fallopian tube is indicated in case of uncontrollable bleeding, irreversibly altered fallopian tubes, or at the patient's request for sterilization. If the contralateral tube is intact, fertility is only minimally impaired.
- Salpingotomy
- Or longitudinal incision of the tube with subsequent removal of the product of conception is chosen especially in the case of ampullary pregnancy. However, the risk of recurrence of GEU in the affected fallopian tube is up to 15%.
- Milking out
- An even more conservative method than salpingotomy, in which the product of conception is removed via the tubal ostia by pressure on the fallopian tube. However, beware of the potential persistence of trophoblast in 5-20% of cases. Suspicion of trophoblast persistence should be considered if there is not a sufficient decrease in serum beta-hCG levels (which is always monitored in the case of treatment of GEU with methotrexate or conservative surgery) or if there is no relapse of symptoms, i.e. pain, bleeding. Methotrexate applied systemically is again used for treatment.
Links[edit | edit source]
External links[edit | edit source]
Literature used[edit | edit source]
- CUNNINGHAM, F. Gary, et al. Williams obstetrics. 23. edition. 2010. ISBN 978-0-07-149701-5.
- BEREK, Jonathan S. Berek and Novak's gynecology. 14. edition. 2007. ISBN 978-0-78176-805-4.