Functional morphology of the kidney
|
This article was marked by its author as Under construction, but the last edit is older than 30 days. If you want to edit this page, please try to contact its author first (you fill find him in the history). Watch the discussion as well. If the author will not continue in work, remove the template Last update: Thursday, 19 Mar 2020 at 11.43 pm. |
The kidneys have multiple functions. They do not only excrete water, electrolytes and metabolic waste products like urea, creatine, uric acid and end products of hemoglobin breakdown(e.g. bilirubin) but they also serve many homeostatic functions.
Kidney Functions[edit | edit source]
- Excretion of metabolic waste products and foreign chemicals
- Regulation of water and electrolyte balance -The intake of these substances must match their excretion
- Regulation of acid-base balance - Kidneys work together with lings and body fluid buffers to control acid-base balance. Kidneys are the only means oof the body which can eliminate acids like sulfuric acid and phosphoric acid.
- Regulation of concentrations of electrolytes and body fluid osmolality
- Regulation of arterial pressure
- Secretion, metabolism, and excretion of hormones(e.g. erythropoietin-regulation of production of red blood cells-erythrocytes)
- Gluconeogenesis - Kidneys are able to synthesize glucose during prolonged periods of fasting from amino acids and other precursors.
Excretion of metabolic wastes and foreign chemicals
• Eliminating metabolic wastes such as: urea (amino acid metabolism), creatinine (muscle creatine),
uric acid (from nucleic acids), bilirubin metabolism products, and metabolites of various hormones.
• The kidneys also eliminate toxins and other foreign substances like drugs, food additives, etc.
Regulation of Water and electrolytes balance and osmolarity.
• Key mechanism of homeostasis. Keeps fluid balance between intake/output of water by adjusting
the volume of urine, maintains proper concentrations of electrolytes by elimination of excesses,
and maintains proper osmolarity in body fluids.
Regulation of Blood pressure
• Elimination of Na+ and water plays a role in long-term regulation of blood pressure.
• The kidney secretes renin. Renin leads to vasoconstriction (angiotensinogen II) and reduces urine
volume (aldosterone).
Regulation of Acid- base balance
• The kidney and the lungs are the key organs in acid-base regulation. The kidney is the only location
that can excrete certain acids (H3PO4,H2SO4). Also the kidney eliminates body fluid buffers.
Regulation of erythropoiesis
• The kidney secretes erythropoietin, which induces erythropoiesis in the bone marrow. Hypoxia is
an important stimulus for erythropoietin secretion.
Activation of Vitamin D
• The kidney hydroxylases vitamin D to its active form (calcitriol). Thus, play an important role in Calcium
absorption in the GIT and for bone structure.
Gluconeogenesis
• Under prolonged fasting conditions, the kidney’s gluconeogenesis ability rivals the liver’s ability.
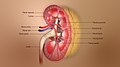
Functional anatomy of the kidney[edit | edit source]
The two kidneys lie on the posterior wall of the abdomen - retroperitoneum space. Each kidney is composed of 8 to 10 lobes and weighs about 150 grams. The medial side of each kidney contains a region called the hilum through which pass the renal artery and vein, lymphatics, nerve supply, and ureter, which carries the final urine from the kidney to the bladder, where it is stored until emptied. The kidney is surrounded by a tough, fibrous capsule that protects its delicate inner structures. The kidney divided into two regions – medulla and cortex. The medulla is divided into multiple cone-shaped masses of tissue called renal pyramids. The base of each pyramid originates at the border between the cortex and medulla and terminates in the papilla, which projects into the space of the renal pelvis, a funnel-shaped continuation of the upper end of the ureter. The outer border of the pelvis is divided into open-ended pouches called major calyces that extend downward and divide into minor calyces, which collect urine from the tubules of each papilla. The walls of the calyces, pelvis, and ureter contain contractile elements that propel the urine toward the bladder, where urine is stored until it is emptied by micturition.
Kidney- blood supply
• Blood flow to the kidney is about 20-25% of the cardiac output at rest (1-1.25 L/min).
• The blood supply of the kidney forms a portal system, a unique vascular arrangement found only
in 3 locations in the body (liver, kidneys, hypophysis).
• Renal portal system (2 capillary beds in series): afferent arteriole -> glomerular capillaries ->
efferent arteriole -> peritubular capillaries -> vasa recta -> interlobular veins.
Basic anatomy of the nephron- the kidney’s functional unit[edit | edit source]
•Uriniferous tubule= nephron + its collecting duct.
• Nephron is the basic functioning unit of the kidney. Each kidney contains about 1-1.5 million
nephrons. Each nephron consists of a renal corpuscle and a renal tubule.
• Each renal corpuscle consists of an anastomosing capillary network called the glomerulus,
surrounded by the glomerular capsule (bowman's capsule).
• The glomerular capsule connects to the renal tubule. The renal tubule can be divided into various
segments.
• There are 2 types of nephrons, cortical nephron and juxtamedullary nephrons. The cortical
nephrons are found more superficially in the cortex, while the juxtamedullary ones are found
next to the corticomedullary junction.
• Both types of nephrons produce urine, but the juxtamedullary nephrons produce more concentrated urine, due to its hypertonic environment.
• The renal tubules can be divided into: proximal convoluted tubule, loop of Henle, distal convoluted tubule and a
connecting tubule.
• Loop of Henle= proximal straight tubule+ thin descending limb + thin ascending limb + distal straight tubule (also thick ascending limb).
• The distal tubule's final part is called the connecting tubule. The connecting tubule connects to the collecting duct.
Physiologic Anatomy of the Kidneys[edit | edit source]
Kidneys lie outside the peritoneal cavity on the posterior wall of the abdomen. Each kidney weighs about 150 grams. There is an indented region at the medial side of each kidney known as hilum. The renal artery and vein, lymphatics, and nerve supply and ureter pass through the hilum. The hilum carries the final urine from the kidney to the bladder. Moreover, there is a capsule surrounding the kidneys. This is a tough, fibrous capsule which protects them and also prevents their expansion.
The kidneys have an outer cortex and an inner medulla region. The medulla has 8-10 renal pyramids (lobes). The loose connective tissue in the medulla allows accumulation of osmotically active substances. The base of each pyramid is at the border between the cortex and the medulla whereas the apex of the pyramid is called a papilla and it projects into the space of the renal pelvis.
References[edit | edit source]
HALL, John. E. Guyton and Hall: Textbook of Medical Physiology. 12th Edition edition. 2011. ISBN 978-1-4160-4574-8.
POKORNY, . Functional Morphology of the Kidney [lecture for subject Physiology, specialization Excretory System, First Faculty of Medicine Charles University]. Prague. 19/02/2013.