Hyperparathyroidism
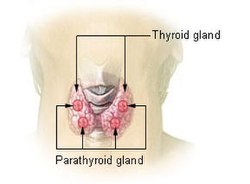
Parathyroid glands are endocrine-active organs whose product is the parathormone. Its function is to regulate calcium metabolism - it has hypercalcemic effects. It acts on bones, where it increases osteoclastic resorption, increases the absorption of calcium in the kidneys and reduces the absorption of phosphates. In the intestines it increases the absorption of vitamin D and in the kidneys its hydroxylation to an active product.
Primary Hyperparathyroidism:
Secondary Hyperparathyroidism:
Tertiary Hyperparathyroidism:
Diseases of the parathyroid glands are divided into hyperfunction (hyperparathyroidism) and hypofunction (hypoparathyroidism).
Primary hyperparathyroidism[edit | edit source]
Primary hyperparathyroidism arises as a result of excessive production of parathyroid hormone and its excessive action on peripheral tissues.
Etiology[edit | edit source]
The most common cause is an adenoma of one of the corpuscles (80%). It is less often a case of primary hyperplasia (15%) and rarely of a carcinoma (1-2%). Related to adenoma, it is also necessary to consider the multiple endocrine neoplasia type I syndrome (MEN-I; primary hyperparathyroidism, tumors of the endocrine pancreas and tumor of the pituitary gland).
Clinical features[edit | edit source]
The disease is often diagnosed accidentally during a laboratory examination. If symptoms do develop, they are mainly manifested by affecting the bones, kidneys and gastrointestinal tract.
Bone manifestation: is manifested by bone pain and pathological fractures. Gradual osteoresorption causes the development of osteoporosis and a specific bone disorder - fibrous osteodystrophy (previously incorrectly referred to as osteitis fibrosa cystica). This is characterized by deposits of subperiosteal bone resorption with a typical "pepper and salt" X-ray picture, with severe involvement even brown tumors (osteoclastomas) arise.
Kidney disorders: typical is nephrolithiasis (calcium-oxalate stones), less often nephrocalcinosis (calcification in the interstitium kidneys). Nephrocalcinosis can lead to renal failure.
Gastrointestinal manifestation: includes more frequent occurrence of acute pancreatitis and peptic ulcer, which have a complicated course. Dyspepsia, nausea, vomiting or constipation may occur.
Cardiovascular symptoms: hypercalcemia causes heart rhythm disorders to cardiac arrest in systole. Arterial hypertension occurs more often.
Psychic and neuromuscular symptoms: weakness, fatigue, personality disorders, depression, muscle weakness.
Diagnostics[edit | edit source]
The basis of the diagnosis is a laboratory examination, which demonstrates hypercalcemia (the norm is 2.2-2.7 mmol/l), hypophosphatemia (the norm is 0 .65–1.65 mmol/l) and an increase in the level of serum PTH. Hyperphosphaturia and hypercalciuria are present.
Densitometry and skiagram of the skull and phalanges will clarify bone involvement. USG is sufficient to examine the kidneys.
To detect and localize a tumor or hyperplastic body, we start with a neck USG supplemented with a scintigraphic examination with 99mTc-MIBI or PET/CT with 11C or 18F by choline.
Differential diagnosis[edit | edit source]
We must distinguish individual etiological causes and primary from secondary and tertiary hyperparathyroidism. Furthermore, we exclude other causes of hypercalcemia: familial benign hypocalciuric hypercalcemia, paraneoplastic production of PTH related peptide/1,25-OH-D/PTH in neoplasia, osteolytic involvement, and others.
Therapy[edit | edit source]
The treatment of first choice is surgical removal of the affected parathyroid gland. If its localization is known, it is possible to choose a minimally invasive approach, otherwise bilateral exploration of the neck is chosen. After removal of the adenoma, the calcium level can be expected to drop to the physiological range within 24-48 hours. If the patient suffered from significant demineralization of the skeleton before the operation, severe hypocalcemia, the so-called hungry bone syndrome, may develop as a result of increased calcium absorption from extracellular fluid of bone tissue. Treatment may require large doses of Ca i.v. . Surgical treatment is successful in 95% of cases.
Medical treatment is used in some cases of mild or subclinical course. Estrogens, bisphosphonates, selective estrogen receptor modulators and recently calcimimetics (e.g. cinacalcet) are used, which activate the calcium sensing receptor and lead to thereby reducing PTH secretion.
Severe hypercalcemia is life-threatening. Its treatment consists mainly of hydration and forced diuresis. Is it possible to i.v. administer bisphosphonates (pamidornate in a dose of 30–90 mg per day in an infusion of 0.9% NaCl solution) or the mentioned calcimimetic. In case of unsuccessful conservative treatment or life-threatening hypercalcemia, we choose hemodialysis.
Secondary hyperparathyroidism[edit | edit source]
It occurs as the body's reaction to hypocalcemia. So it is a physiological reaction. In the laboratory findings low calcemia and high levels of parathyroid hormone are found. There are many causes of secondary hyperparathyroidism, for example: chronic renal failure, reduced absorption of vit. D due to intestinal inflammations, dietary deficiency of vit. D or calcium etc.
Tertiary hyperparathyroidism[edit | edit source]
It arises during long-term secondary hyperparathyroidism, when there is hyperplasia of one or more bodies and autonomous secretion of PTH. Laboratory findings include hypercalcemia and elevated PTH levels.
Understanding Hyperparathyroidism - YouTube
Odkazy[edit | edit source]
Související články[edit | edit source]
References[edit | edit source]
- ČEŠKA, Richard, Tomáš ŠTULC a Vladimír TESAŘ, a Milan LUKÁŠ, et al.. Interna. 3.. edition. Praha : Stanislav Juhaňák - Triton, 2020. ISBN 978-80-7553-780-5.
- GREENSPAN, Francsi S – BAXTER, J. D. Základní a klinická endokrinologie. 1. edition. Praha : H & H, 2003. pp. 843. ISBN 80-86022-56-0.