Kidney - description, position, syntopy (draw scheme), birth defects
From WikiLectures
Kidneys: Description, Position, Syntopy, and Birth Defects
General Description
The kidneys are bean-shaped retroperitoneal organs essential for homeostasis. They filter blood, excreting waste (urea, creatinine) while maintaining electrolyte balance, acid-base equilibrium, and fluid levels. Each kidney regulates blood pressure via the renin-angiotensin-aldosterone system (RAAS) and supports red blood cell production by releasing erythropoietin.
- Location:Retroperitoneally between the T12–L3 vertebrae, with the right kidney slightly lower due to the liver.
- Size & Shape:~10 cm long, ~5 cm wide, and ~3 cm thick. They are reddish-brown with a smooth outer surface.
- Superior poles: T12 level.
- Inferior poles: L3 level.
- Hilum: At the L1–L2 level.
- Capsule and Surrounding Structures:
- Renal Capsule: A tough collagenous layer firmly attached to the kidney.
- Perirenal Fat: Surrounds the kidney and acts as cushioning.
- Renal Fascia: Encases the perirenal fat and suprarenal glands, providing stability.
- Pararenal Fat: Lies outside the renal fascia as additional cushioning.
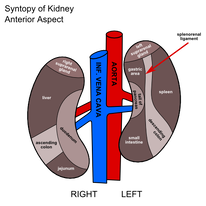
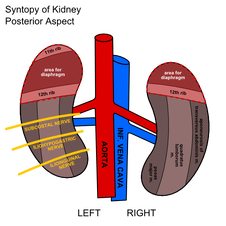
Position and Syntopy
Right Kidney
- Superiorly: Liver (separated by the hepatorenal recess), right adrenal gland.
- Anteriorly: Duodenum, hepatic flexure of the colon.
- Posteriorly: Diaphragm, 12th rib, quadratus lumborum, psoas major, and transversus abdominis muscles.
- Medially: Inferior vena cava (IVC), renal vessels, ureter.
Left Kidney
- Superiorly: Stomach, spleen, left adrenal gland, pancreas (tail).
- Anteriorly: Jejunum, splenic flexure of the colon.
- Posteriorly: Diaphragm, 11th and 12th ribs, quadratus lumborum, psoas major, transversus abdominis muscles.
- Medially: Abdominal aorta, renal vessels, ureter.
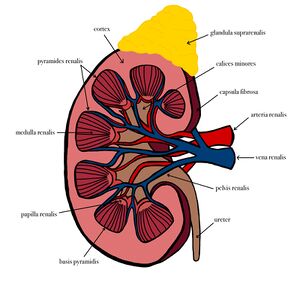
Internal Structure
- Renal Cortex:
- Lies directly beneath the renal capsule.
- Contains glomeruli (site of filtration), proximal and distal convoluted tubules.
- Extensions between the pyramids form renal columns, supporting blood vessels.
- Renal Medulla:
- Comprises 8–12 renal pyramids.
- Pyramids: Base faces the cortex; apex (papilla) points toward the renal sinus.
- Zones:
- Outer striated zone.
- Inner pale zone.
- Contains loops of Henle and collecting ducts for urine concentration.
- Renal Sinus:
- Central cavity housing:
- Renal pelvis.
- Major and minor calyces.
- Renal vessels, lymphatics, and nerves.
- Adipose tissue for cushioning.
- Central cavity housing:
- Renal Pelvis & Calyces:
- Renal Pelvis: Funnel-shaped origin of the ureter, which collects urine.
- Major Calyces: Divide into 2–3 branches.
- Minor Calyces: Surround renal papillae, collecting urine from each pyramid.
Vascular Supply and Lymphatics
- Arterial Supply:
- Renal Arteries: Arise from the abdominal aorta at L1–L2.
- Divide into 5 segmental arteries: Superior (apical), anterior superior, anterior inferior, inferior, and posterior.
- Branching pattern:
- Segmental → Interlobar → Arcuate → Cortical radiate arteries.
- Some cortical radiate arteries perforate the renal capsule to supply the perirenal tissues.
- Renal Arteries: Arise from the abdominal aorta at L1–L2.
- Venous Drainage:
- Renal veins drain into the inferior vena cava (IVC).
- Left Renal Vein: Longer than the right, receiving tributaries from the left gonadal vein, left suprarenal vein, and sometimes the phrenic vein.
- Lymphatic Drainage:
- Follows renal veins to lumbar (caval and aortic) lymph nodes.
Ureter and Associated Structures
- Description:
- 25–30 cm long muscular tubes transporting urine from kidneys to the bladder.
- Diameter: ~4–7 mm.
- Constricted at three points:
- Ureteropelvic junction.
- Crossing of iliac vessels.
- Ureterovesical junction (entry into bladder).
- Blood Supply:
- Abdominal Ureter: Supplied by renal arteries, abdominal aorta, and gonadal arteries.
- Pelvic Ureter: Supplied by superior vesical, middle rectal, and inferior vesical/uterine arteries.
Functional Highlights
- Filtration: Occurs in the glomeruli. Ultrafiltrate is processed to form urine.
- Reabsorption and Secretion: Occurs in the tubules for electrolyte and water balance.
- Concentration of Urine: Managed by the loop of Henle and collecting ducts.
Birth Defects and Anomalies
- Renal Agenesis:
- Absence of one (unilateral) or both (bilateral) kidneys. Bilateral agenesis is incompatible with life.
- Horseshoe Kidney:
- Inferior poles of kidneys fuse across the midline. Often asymptomatic but may cause obstruction or infections.
- Ectopic Kidney:
- Kidney fails to ascend during development, often located in the pelvis.
- Polycystic Kidney Disease (PKD):
- Autosomal dominant or recessive disorder causing numerous cysts, leading to kidney enlargement and dysfunction.
- Duplex Kidney:
- A single kidney with two ureters or a duplicated renal pelvis.
- Pelvic Kidney:
- A kidney that remains in the pelvis due to developmental failure to ascend.
- Multicystic Dysplastic Kidney (MCDK):
- Non-functional kidney with multiple cysts due to disrupted nephron development.
- Wilms Tumor:
- Congenital malignancy affecting children under five, arising from primitive renal tissue