Metabolism of purine nucleotides, regulation, inhibitors, disorders.
Atoms of the purine ring are composed of compounds that include amino acids (aspartic acid, glycine and glutamine), CO2 and N10-formyltetrahydrofolate.
Synthesis[edit | edit source]
The purine ring is formed mainly in the liver in a sequence of reactions in which carbon and N atoms are added to the already formed ribose-5-phosphate, which comes from the pentose cycle.
5-phosphoribosyl-1-pyrophosphate (PRPP) is an "activated pentose" involved in the synthesis and salvage pathway of purines and pyrimidines.
Synthesis of PRPP from ATP and ribose-5-phosphate is catalyzed by PRPP synthase (ribose phosphate pyrophosphate knase).
- This X-linked enzyme is activated by inorganic phosphate and inhibited by purine nucleotide (feedback inhibition by product).
The sugar component of PRPP is ribose and therefore ribonucleotides will be the final product of de novo purine synthesis. In order to create the deoxyribonucleotides needed for DNA synthesis, the ribose part is reduced.
Synthesis of 5'-phosphoribosylamine from PRPP and glutamine is the next step in purine synthesis. The amide group of glutamine replaces the pyrophosphate group attached to carbon #1 in PRPP.
- The enzyme catalyzing the glutamine phosphoribosylpyrophosphate amidotransferase reaction is inhibited by the purine nucleotides AMP and GMP – the end products of this metabolic pathway.
- The reaction is activated by the intracellular concentration of PRPP.
Another 9 steps of purine nucleotide biosynthesis lead to inosine monophosphate (IMP).
This pathway requires ATP as an energy source and 2 intermediate steps require N10-formyltetrahydrofolate.
- Certain synthetic inhibitors of purine synthesis (eg sulfonamides) are intended to inhibit the growth of rapidly multiplying microorganisms without affecting human bb. Other inhibitors of purine synthesis, such as folic acid analogues (eg methotrexate), are used pharmacologically to stop the spread of cancer by inhibiting the synthesis of nucleotides and thus DNA and RNA.
- Inhibitors of human purine synthesis are extremely toxic to various tissues, especially to developing fetal structures or rapidly proliferating cells, such as in the bone marrow, skin, GIT, immune system or hair follicles. Because of this, people taking anti-cancer therapy may experience side effects such as anemia, scaly skin, digestive disorders, immunodeficiency, and hair loss
The conversion of IMP to AMP or GMP represents a two-step, energy-intensive metabolic pathway. AMP synthesis requires GTP as an energy source, while GMP synthesis uses ATP.
The first reaction of each pathway is inhibited by its end product. This represents a mechanism to direct the conversion of IMP to more required nucleotides. If AMP and GMP are present in sufficient quantities, purine synthesis is again stopped at the aminotransferase step.
Nucleoside diphosphates are synthesized from the respective nucleoside monophosphates using specific nucleoside monophosphate kinase. These kinases distinguish the sugar component of nucleotides.
ATP is a general source of added phosphates, as it is found in cells in higher concentrations than other nucleoside triphosphates.
Adenylate kinase is active mainly in the liver and muscle, where ATP is an important source of energy. The function of this enzyme is to maintain the balance between AMP, ADP and ATP.
Nucleoside diphosphates and triphosphates are converted into each other by nucleoside diphosphate kinase – an enzyme which, unlike monophosphate kinase, has a broad specificity.
Salvage pathway[edit | edit source]
Purines released by the normal breakdown of nucleic acids in cells, or those originating in small amounts in the diet and not degraded, can be converted to nucleoside triphosphates and used in the body. This process is referred to as the "rescue or sparing pathway" for purines.
2 enzymes are involved in the conversion of purine bases into nucleotides:
- adenine phosphoribosyltransferase (APRT)
- hypoxanthine-guanine phosphoribosyltransferase (HGPRT)
Both enzymes use PRPP as a source of ribose-5-phosphate group.
Release of pyrophosphate and its subsequent hydrolysis by pyrophosphatase make these reactions irreversible.
Adenosine is the only nucleoside that undergoes a salvage pathway. It is subsequently phosphorylated to AMP by adenosine kinase.
All nucleotides described so far contained ribose as a sugar component (ribonucleotides). However, the nucleotides required for DNA synthesis are 2'-deoxyribonucleotides, produced from ribonucleoside diphosphates by the enzyme ribonucleotide reductase during the S-phase of the cell cycle.
Ribonucleotide reductase (ribonucleoside diphosphate reductase) is an enzyme from two non-identical dimer subunits, R1 and R2, and is specific for the reduction of purine nucleoside diphosphates (ADP and GDP) and pyrimidine nucleoside diphosphates, cytidine diphosphate (CDP) and uridine diphosphate (dP ).
- The donor of the proton needed for the reduction of the 2'-hydroxyl group is the 2 sulfhydryl groups of the enzyme, which form disulfide bridges during the reduction.
- In order for ribonucleotide reductase to continue producing deoxyribonucleotides, the disulfide bond formed during the formation of the 2'-deoxy carbon must be reduced.
- The source of reducing equivalents for this purpose is thioredoxin – a peptide coenzyme of ribonucleotide reductase. Thioredoxin contains 2 cysteine residues separated by 2 amino acids in the peptide chain
Two sulfhydryl groups of thioredoxin supply its hydrogen atoms to ribonucleotide reductase, in the process of forming a disulfide bridge.
- Thioredoxin must be converted back to its reduced form in order to continue its activity.The necessary reduction coefficients are provided by NADPH + H+ and the reaction is catalyzed by thioredoxin reductase.
Ribonucleotide reductase is responsible for maintaining a balanced supply of deoxyribonucleotides for DNA synthesisn In order to achieve this, the regulation of the enzyme must be complex.
- In addition to active sites, allosteric sites are also involved in enzyme regulation.
- The binding of dATP to the allosteric sites of the enzyme inhibits its overall catalytic activity and thus prevents the reduction of nucleotide diphosphates. This effectively prevents DNA synthesis and explains the toxicity of increased dATP levels as a result of e.g. deficiency of adenosine deaminase
- Conversely, the binding of ATP to these sites activates the enzyme.
- The binding of nucleotide triphosphates to the substrate specific sites of the enzyme regulates the substrate specificity, which increases the conversion of various types of ribonucleotides to deoxyribonucleotides, which are important for DNA synthesis.
- For example binding of deoxythymidine triphosphate (dTTP) to a site-specific substrate causes a conformational change that allows the reduction of GDP to dGDP at the catalytic site.
Degradation[edit | edit source]
Degradation of nucleic acids from food takes place in the small intestine, where a family of pancreatic enzymes hydrolyze nucleic acids into nucleotides.
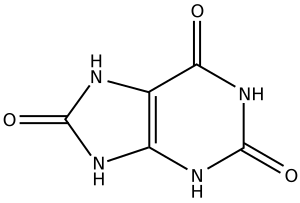
In the mucosal cells of the small intestine, purine nucleotides are gradually degraded by specific enzymes to nucleosides and free bases, and subsequently to uric acid as the end product of this pathway.
Purine nucleotides from de novo synthesis are degraded primarily in the liver. Free bases from this degradation undergo a sparing pathway and are transported from the liver to peripheral tissues.
Ribonucleases and deoxyribonucleases secreted by the pancreas hydrolyze DNA and RNA in food into oligonucleotides. Oligonucleotides are further hydrolyzed by pancreatic phosphodiesterases, resulting in a mixture of 3'- and 5'-mononucleotides.
In the intestinal mucosa, a family of nucleotidases hydrolytically removes phosphate groups, thereby releasing nucleosides, which are further degraded to free bases.
Purine bases from the diet are not used for NK synthesis, but are instead converted to acid. urine in the intestinal mucosa.
Most uric acid enters the blood and is subsequently excreted in the urine. In other mammals, except subhuman primates, they convert the purine ring into allantoin using urate oxidase.
Uric acid is produced by subsequent reactions:
- An amino group is removed from AMP to form IMP by AMP deaminase or from adenosine to form inosine (hypoxanthine ribose) by adenosine deaminase.
- IMP and GMP are converted to their nucleotide forms – inosine and guanosine by means of 5'-nucleotidase.
- Purine nucleoside phosphorylase converts inosine and guanosine to the free purine bases, hypoxanthine and guanine. Mutase converts ribose-1-phosphate to ribose-5-phosphate.
- Guanine is deaminated to xanthine.
- Hypoxanthine is oxidized by xanthine oxidase to xanthine, which is subsequently oxidized by xanthine oxidase to uric acid, the end product of purine degradation in humans. Uric acid is excreted in the urine.
Pathobiochemistry[edit | edit source]
Lesch-Nyhan syndrome[edit | edit source]
Lesch-Nyhan syndrome is a rare X-linked recessive disorder associated with virtually complete deficiency of HGPRT. This deficiency causes the inability of the salvage pathway for hypoxanthine or guanine, resulting in the formation of large amounts of uric acid, the end product of purine degradation. In addition, failure of the rescue pathway causes increased PRPP levels and decreased IMP and GMP levels.
As a result, glutaminephosphorybosylphosphate aminotransferase has an excess of substrate and a reduced amount of inhibitors, and therefore purine synthesis is de novo increased. The combination of reduced purine reutilization and increased purine synthesis causes increased purine degradation and production of large amounts of uric acid leading to hyperuricemia, which causes the formation of uric acid stones in the kidneys (urolithiasis) and the deposition of uric acid crystals in the joints (gouty arthritis) and soft tissues. In addition, the syndrome is characterized by motor dysfunction, cognitive deficits, and behavioral disturbances that include self-injury (eg, lip and finger biting).
Gout[edit | edit source]
Gout is a disorder characterized by high levels of uric acid in the blood (hyperuricemia), as a result of either overproduction or insufficient excretion of uric acid. Hyperuricemia can lead to the deposition of sodium urate crystals in the joints and an inflammatory reaction to them, causing first acute and then chronic gouty arthritis. Sodium urate crystals (tophi) can settle in the soft tissues and cause chronic tophitic gout there. The formation of stones from uric acid in the kidneys (urolithiasis) may also occur. Hyperuricemia is often asymptomatic and does not lead to gout, but gout is accompanied by hyperuricemia.
Definitive diagnosis of gout requires collection and examination of synovial fluid from the affected joint or affected tissue using light microscopy to confirm the presence of uric acid crystals. In the vast majority of patients with hyperuricemia leading to gout, this condition is caused by insufficient excretion of uric acid. Insufficient excretion can be caused firstly by an unknown hereditary disorder of excretion and secondly by known disease processes that affect the excretion of uric acid by the kidneys (e.g. in lactic acidosis – lactate and uric acid have the same renal transporter, which compete with each other) and external factors such as medication use (eg. thiazide diuretics) or after lead poisoning (saturinine gout).
A less common cause of gout is hyperuricemia caused by overproduction of uric acid. In most cases, primary hyperuricemia is idiopathic (of unknown cause). However, several identified mutations in the X-linked PRPP synthase gene that cause increased Vmax for PRPP production and lower Km for ribose 5-phosphate or reduced sensitivity to purine nucleotide-allosteric inhibitors. In any case, an increased concentration of PRPP accelerates production of purines, causing elevated plasma uric acid levels.
Sources[edit | edit source]
MATOUŠ, Bohuslav, et al. Základy lékařské chemie a biochemie. 1. vydání. Praha: Galén, 2010. 540 s.