Uterine (Fallopian) Tube - Structure, Divisions, Position, and Vascular Supply
Uterine (Fallopian) Tube - Structure, Divisions, Position, and Vascular Supply
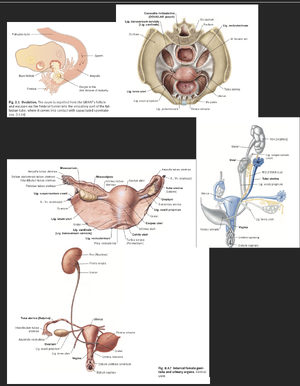
The uterine (Fallopian) tube is a paired structure that serves as the conduit for the transport of ova from the ovary to the uterus. It is also the site of fertilization. Below is a detailed explanation based on Gray’s Anatomy and Sobotta Atlas of Human Anatomy.
1. Structure of the Uterine Tube
The uterine tube is approximately 10–12 cm long and has a lumen lined with mucosa, surrounded by muscular and serosal layers:
1. Mucosa:
a. Lined with ciliated columnar epithelium and secretory cells.
b. The cilia beat towards the uterus, aiding in the movement of the ovum or fertilized egg.
2. Muscularis:
a. Composed of inner circular and outer longitudinal smooth muscle layers, which facilitate peristaltic contractions.
3. Serosa:
a. The outermost layer derived from the peritoneum.
2. Divisions of the Uterine Tube
The uterine tube is divided into four main regions:
1. Infundibulum:
a. The funnel-shaped distal end near the ovary.
b. Possesses finger-like projections called fimbriae, which help capture the ovulated oocyte.
c. The ostium is the opening into the peritoneal cavity.
2. Ampulla:
a. The widest and longest portion of the tube.
b. This is the most common site of fertilization.
3. Isthmus:
a. A narrow, thick-walled portion near the uterus.
b. It serves as a transitional zone between the ampulla and the uterine part.
4. Uterine (Intramural) Part:
a. The segment that passes through the uterine wall.
b. Opens into the uterine cavity at the uterine ostium.
3. Position of the Uterine Tube
1. Location:
a. Situated in the upper border of the broad ligament (mesosalpinx), a double fold of peritoneum.
2. Relation to Other Structures:
a. Lateral end (infundibulum) lies close to the ovary but is not directly attached, leaving a communication between the peritoneal cavity and the uterine cavity.
b. Medial end connects to the uterine cavity at the uterine horn.
1. Vascular Supply
a. Arterial Supply:
i. Tubal branches of the ovarian artery (from the abdominal aorta).
ii. Tubal branches of the uterine artery (from the internal iliac artery).
iii. These two sources form an anastomotic network along the mesosalpinx.
b. Venous Drainage:
i. Drains into the ovarian veins (to the inferior vena cava or left renal vein) and the uterine veins (to the internal iliac vein).
c. Lymphatic Drainage:
i. Lymph flows to the lumbar lymph nodes and internal iliac lymph nodes.
d. Innervation:
i. Sympathetic innervation is derived from the ovarian plexus.
ii. Parasympathetic innervation comes from the pelvic splanchnic nerves (S2–S4).
Clinical Correlations
1. Ectopic Pregnancy:
D. Most ectopic pregnancies occur in the ampulla.
E. It is a life-threatening condition if the tube ruptures.
2. Pelvic Inflammatory Disease (PID):
a. Infection can damage the cilia or cause scarring, leading to infertility or increased risk of ectopic pregnancy.
3. Surgical Relevance:
a. Tubal ligation is a common contraceptive procedure where the tubes are surgically blocked.
The uterine tube is a vital structure in the female reproductive system, functioning as the site of fertilization and the pathway for gamete transport. Its anatomical positioning and vascular supply underline its role in both physiology and pathology.