Vascualr supply of kideny, segments
From WikiLectures
Vascular Supply of the Kidney[edit | edit source]
The kidneys are highly vascularized organs, receiving 20–25% of cardiac output to facilitate filtration and maintain homeostasis. The vascular anatomy is segmental, reflecting their functional units.
Detailed Arterial Supply of the Kidney:[edit | edit source]
- Renal Artery:
- The renal artery is a large branch of the abdominal aorta, typically arising at the level of L1-L2 vertebrae.
- Right renal artery is longer than the left because the aorta is positioned to the left of the midline.
- Renal arteries are often slightly variable, with some individuals having accessory renal arteries that supply additional parts of the kidney, particularly the lower pole.
- Segmental Arteries:
- Upon entering the kidney at the hilum, the renal artery divides into segmental arteries (usually 5 in number):
- Apical (superior) segmental artery: Supplies the upper pole.
- Anterosuperior segmental artery: Supplies the anterior superior region of the kidney.
- Anteroinferior segmental artery: Supplies the anterior inferior region.
- Inferior segmental artery: Supplies the lower pole.
- Posterior segmental artery: Supplies the posterior region.
- These segmental arteries are important because each segment of the kidney is functionally and surgically independent. If one segment becomes damaged or needs to be resected (e.g., in the case of kidney surgery), the blood supply to other segments remains unaffected.
- Upon entering the kidney at the hilum, the renal artery divides into segmental arteries (usually 5 in number):
- Interlobar Arteries:
- After the segmental arteries enter the renal parenchyma, they pass through the renal columns (between the renal pyramids) as interlobar arteries.
- These arteries then ascend toward the renal cortex and give rise to arcuate arteries at the corticomedullary junction.
- Arcuate Arteries:
- The arcuate arteries run along the corticomedullary junction, where the cortex meets the medulla.
- They give rise to smaller interlobular (cortical radiate) arteries, which are crucial for supplying the renal cortex.
- Interlobular (Cortical Radiate) Arteries:
- These arteries branch from the arcuate arteries and extend toward the kidney cortex.
- At the cortex, they further branch into afferent arterioles, which then lead to the glomerular capillaries, where filtration takes place.
- Juxtamedullary Nephrons:
- Some afferent arterioles enter the juxtamedullary nephrons, which are located near the medulla. These arterioles are associated with the vasa recta, a specialized network that supplies the medulla, crucial for concentrating urine.
Venous Drainage:[edit | edit source]
- Cortical Radiate Veins (Interlobular Veins):
- The cortical radiate veins collect deoxygenated blood from the cortex and drain into the arcuate veins.
- Arcuate Veins:
- The arcuate veins are responsible for draining the blood from the arcuate arteries at the corticomedullary junction.
- These veins converge into the interlobar veins, located between the renal pyramids.
- Interlobar Veins:
- The interlobar veins drain into the renal vein at the hilum of the kidney.
- Renal veins are important for returning blood to the inferior vena cava.
- Renal Vein:
- The renal veins drain deoxygenated blood from the kidney.
- The left renal vein is longer than the right and crosses anterior to the aorta.
- The right renal vein is shorter and drains directly into the inferior vena cava.
Additional Relevant Topics:[edit | edit source]
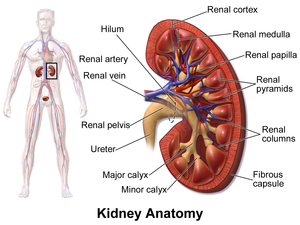
- Renal Hilum and Renal Capsule:
- The renal hilum is the entry and exit point for the renal arteries, veins, and ureters.
- The renal capsule is a fibrous covering of the kidney that provides protection.
- Renal Medulla and Cortex:
- The renal cortex contains the glomeruli, which perform filtration.
- The renal medulla consists of renal pyramids that contain the loop of Henle and the vasa recta.
- The vasa recta supplies oxygen to the medulla and plays a role in countercurrent exchange, aiding in urine concentration.
- Clinical Considerations:
- Renal Artery Stenosis: A narrowing of the renal arteries that may lead to hypertension.
- Renal Infarction: Occurs when blood supply to a kidney segment is blocked, usually by a clot or embolism.
- Transplantation: Renal transplant surgeons must be cautious about vascular variations, such as accessory renal arteries, to ensure proper blood supply after grafting.
- Accessory Renal Arteries:
- These are extra arteries that may originate from the abdominal aorta or other vessels like the iliac artery and supply the kidney.
- They are clinically significant because they may be accidentally damaged during surgeries, leading to ischemia in certain parts of the kidney.
- Lymphatic Drainage:
- Lymph from the kidney drains into lumbar (lateral aortic) lymph nodes, which are located near the origin of the renal arteries.
- These nodes are connected to the cisterna chyli and ultimately drain into the thoracic duct.
Clinical Correlations[edit | edit source]
- Renal Artery Stenosis
- Narrowing of the renal artery leads to reduced blood flow, triggering hypertension through the renin-angiotensin-aldosterone system.
- Segmental Infarction
- Due to the absence of significant collateral blood supply, blockage in a segmental artery may lead to localized kidney infarction.
- Accessory Renal Arteries
- Present in approximately 25% of individuals and may supply the lower or upper pole of the kidney. These are remnants of embryological development and are clinically significant in surgeries like nephrectomy or renal transplantation.
- Renal Vein Thrombosis
- Common in hypercoagulable states, leading to flank pain, hematuria, and reduced kidney function.