Cardiac catheterization
Left cardiac catheterization[edit | edit source]
Left-sided cardiac catheterization is the most accurate method of coronary heart disease (CHD).
- Most often under sciascopic control retrogradely through the aorta and it's branches
- Under local anesthesia we puncture the femoral artery or radial artery → we insert the guidewire and the introducer (Seldinger's technique) → we insert our own diagnostic catheters through the introducer into the distance of the coronary artery dextra et sinistra + into the left ventricle
- Unusually left-sided transseptal catheterization: the catheter is introduced through the femoral vein into the right atrium → we puncture the inter atrial septum and we penetrate the left atrium into the left atrium or left ventricle
- Left heart catheterization includes:
- Selective coronarography + left ventriculography – coronary artery injection + left ventricle with X-ray contrast agent
- Tonometry – measurement of pressures in the left ventricle + in the aorta, determination of pressure gradients through the mitral + aortic valve
- Oxymetry – taking blood from individual sections of the heart (determination of blood oxygen saturation) to detect short circuits
Coronary angiography[edit | edit source]
- Widely used method to assess coronary artery/ coronary artery bypass grafting
- We determinace the degree of narrowing of the coronary artery - in % (lumen of the artery in the narrowed area / in the nearest unaffected area)
- A narrowing of >50% is significant
- We also assess: type of stenoses, presence of collaterals, calcifications, developmental abnormalities
- Indications: suspicion of severe coronary artery disease, assessment + differential diagnostic reasons after heart transplantation
- Relative contraindications: Active infection, severe anemia, disruption of the internal environment, severe uncontrollable hypertension, bleeding, severe blood clotting disorders, patient disapproval of revascularization
Left ventriculography[edit | edit source]
- We determine the regional and global systolic function of the left ventricle
- Currently it can be replaced by ECHO → we perform it only in connection with selective coronarography
- Evaluation of momentum of individual parts of the left ventricle:
- Normokinesis (normal contractility),
- Hypokinesia,
- Akinesia (the monitored part of the left ventricle does not contract),
- Dyskinesia (abnormal arching of part of the left ventricular wall during systole),
- Ejection fraction (EF) – it expresses the global systolic function of the left ventricle; standard: >55%
- EF = (EDV – ESV) / EDV. 100%.
Complications of left heart catheterization[edit | edit source]
- Local: haemorrhage, hematoma, pseudoaneurysm, arteriovenous fistula at the femoral artery
- Cardiac and general: AIM, heart failure, arrhytmias, stroke, vagal reactions (hypotension+ bradykardia).
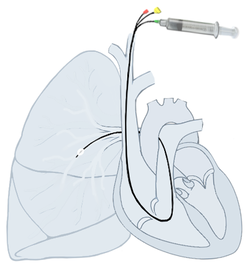
Right cardiac catheterization[edit | edit source]
For pressure monitoring in the pulmonary artery we use a special floating balloon Swan-Ganza catheter. It is inserted through the right heart into the lungs and wedged in one of its branches by an inflated balloon. Modern catheters are able to measure multiple parameters: central venous pressure, the right atrial pressure, right ventricular pressure and the pulmonary artery pressure. Indications have recently been limited due to the possibility of detecting many cardiovascular parameters mainly through ultrasonography. The measurement of wedge pressure is crucial, because it is not detectable in any other way. Right-sided cardiac catheterization can also be used for differential diagnosis and definitive confirmation of the diagnosis of pulmonary hypertension.
Parameters directly measurable:
- pulmonary artery pressure, central venous pressure,
- pulmonary capillary wedge pressure,
- cardiac output,
- saturation of mixed vein blood,
- central body temperature.
Additional circulatory parameters can be calculated from the measured parameters:
- systemic and pulmonary vascular resistance,
- stroke volume,
- oxygen consumption and supply,
- left ventricular and right ventricular labour index.
Pulmonary hypertension[edit | edit source]
Catheterization allows measurement of pressure levels in the pulmonary and comparison with wedge pressure, which makes it possible to distinguish between the precapillary and postcapillary causes of pulmonary hypertension. By definition, pulmonary hypertension is considered to be mean pulmonary artery pressure > 25 mm Hg.
Pulmonary Capillary Wedge Pressure[edit | edit source]
Pulmonary Capillary Wedge Pressure (PCWP) is the pressure in the final branch of the lung after being sealed with a balloon. After stopping the inflow from pulmonary artery, the pressures equalize and its pressure should be equal to the pressure in the left atrium and thus represent some of the functions of the left heart. The standard is 2-12 mmHg.[1] Pressure varies depending on the heart cycle similar to a phlebogram. The pressure level is used to assess the left heart filling (preload) and hydrostatic pressure in the pulmonary capillaries.
Increased PCWP is associated with conditions that increase left ventricular end-diastolic pressure - left-sided heart failure both systolic and diastolic, mitral and aortic valve defects, hypertrophic, constrictive and restrictive cardiomyopathy, hypervolaemia, right-left short circuits, or cardiac tamponade.
Decreased PCWP is present in hypovolemia, pulmonary veno-occlusive disease or massive pulmonary embolism.
Other measured parameters[edit | edit source]
These measured parameters can now usually be replaced by ultrasonography or other non-invasive methods.
Measuring minute cardiac output (CO)[edit | edit source]
- blood volume expelled by the heart into circulation in 1 minute,
- normal: 4–8 l/min,
- cardiac index: 2,5–4,5 l/min/m2 of body surface area,
- can be measured in multiple ways:
Thermodilution[edit | edit source]
- With a floating Swan-Ganz catheter inserted, with a thermistor at the end
- inject 10 ml of room temperature saline (approx. 18-22 °C) through the proximal hole in the catheter,
- the distal thermistor shows a curve that results from a change in ambient blood temperature over time,
- minute volume smaller → applied solution flows past the thermistor slower → temperature difference is smaller + area under curve larger.
Dilution method by dye indicator[edit | edit source]
- Determination of the volume of fluid according to the concentration of the indicator (usually in the peripheral artery), a known amount of which has been dissolved in the fluid.
Fick´s principle[edit | edit source]
- The volume of blood that flows through the lungs per minute = cardiac output per minute,
- value given: (patient oxygen consumption/min) / (arterial blood oxygen content - mixed venous blood oxygen content)
Vascular resistance measurement[edit | edit source]
Vascular resistance is based on Ohm's Law: ratio of pressure gradient + flow rate().
Pulmonary vascular resistance (PVR)[edit | edit source]
- Normal: 20–130 dyn/s/cm-5,
- ,
- (TPG: transpulmonary gradient; MSV: minute cardiac output; PAP: medium pressure in the lung; PLS: medium pressure in the left atrium, resp. pulmonary capillary wedge pressure),
- is determined mainly before cardiac surgery (short-term defects, heart transplantation).
Peripheral (systemic) vascular resistance (SVR)[edit | edit source]
SVR:
- Normal: 700–1600 dynes/s/cm-5,
- ,
- (PAO: medium pressure in the aorta; PPS: medium pressure in the right atrium; MSV: minute cardiac output),
- importance in heart failure (decrease may lead to improvement).
References[edit | edit source]
Related articles[edit | edit source]
References[edit | edit source]
- DÍTĚ, P.. Internal medicine. 2. edition. Praha : Galén, 2007. ISBN 978-80-7262-496-6.
- ↑ 1 ŠEVČÍK, Pavel, et al. Intenzivní medicína. 3. vydání. Galén, 2014. 1195 s. s. 157–161. ISBN 9788074920660