Drug delivery routes into the body
The delivery routes are the gates through which the drug enters the body. Even at the level of administration, interactions between different drugs can occur. If there is an interaction due to physico-chemical and chemical properties, it is a pharmacological interaction, if there is an interaction at the level of specific structures, it is a pharmacokinetic interaction. The actual choice of the route of administration is determined by consideration of possible interactions, the possibility of cooperation with the patient and, last but not least, the properties of the drug itself.
Overview of the most common routes[edit | edit source]
- system application
-
- enteral application – absorption of the medicine occurs mainly through the GIT
- oral
- rectal
- (sublingual and buccal)
- parenteral application – absorption bypasses the GIT
- injectable
- intravenous
- intramuscular
- subcutaneous
- intradermal
- intra-arterial
- intracardiac
- intrathecal
- into the bone marrow (intraosseous)
- inhalation
- transdermal
- injectable
- enteral application – absorption of the medicine occurs mainly through the GIT
- local application
-
- on the skin
- on mucous membranes
- on the mucous membranes of the GIT (the drug is not absorbed)
Sublingual and buccal administration[edit | edit source]
With this administration, the substances pass into the systemic circulation through the well-perfused mucous membrane of the oral cavity. Lipophilic substances are better absorbed. Because the blood does not flow directly into the portal basin, the first-pass effect is significantly suppressed. The effect usually occurs within 15 minutes. The condition for administration is sufficient hydration and cooperation of the patient. Not suitable for unpleasant tasting and irritating substances.
Pharmaceutical forms can be, for example, lingvets' (sublingual tablets), lollipops' (e.g. fentanyl), porous sugar cubes''' (e.g. tramadol , ketamine, midazolam, neostigmine) or sprays' (glycerol trinitrate).
Oral administration[edit | edit source]
When administered orally, absorption occurs mainly through the mucosa of the small intestine. Some substances acting locally in the digestive tract are also administered orally, e.g. carbo medicinalis, bulk laxatives or mesalazine. The systemic effect of orally administered drugs usually occurs within 30 minutes, but controlled-release preparations are also produced. The so-called 'therapeutic systems release the active substance slowly during passage through the intestine, enteric-soluble tablets protect sensitive substances from the acidic environment of the stomach. After absorption, the substance passes through the liver and a significant first-pass effect can occur, i.e. a significant metabolic interaction with liver enzymes. Bioavailability can change depending on food intake, activity of digestive processes, intestinal motility, etc.
The main disadvantages of oral administration of drugs are:
- variability in bioavailability between and within individuals,
- slow onset of effect,
- generally more problematic interchangeability of preparations with the same active substance from different manufacturers.
Rectal administration[edit | edit source]
Medicines can be administered rectally in the form of suppositories or solutions. Can also be used on unconscious patients. There is less inter-individual variation in bioavailability with rectal administration compared to oral administration. Part of the blood from the rectum drains into the v. cava inf., so the first‑pass effect is less pronounced. The effect usually starts within 15-20 minutes. Cannot be administered in case of inflamed mucous membrane. Systemically acting substances (analgesics, ethyl alcohol) and locally acting substances (mesalazine) can be given. Absorption is often incomplete and irregular. Many medications can also irritate the rectal mucosa.
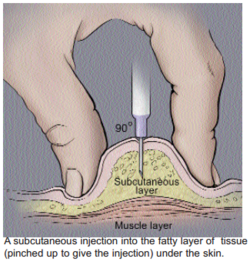
Subcutaneous administration[edit | edit source]
After subcutaneous administration, lipophilic and hydrophilic substances are quickly absorbed, but the onset is slower than with intramuscular application. A depot can also be created, for example a sterile pellet releasing a contraceptive can be implanted subcutaneously. Subcutaneous administration is possible only when applying non-irritating drugs.
Intramuscular administration[edit | edit source]
Both hydrophilic and hydrophobic substances can be administered in greater amounts than subcutaneous administration. The effect starts within 15-20 minutes. But the speed depends on the type of muscle and fat storage. Mildly irritating substances can also be administered, depots can be created. Not every drug can be administered intramuscularly. i.m. are not served:
- medicines, the application of which would be significantly painful (iron preparations, quinolone chemotherapy),
- some non-steroidal anti-inflammatory substances (risk of sterile abscesses),
- anticoagulant or thrombolytic agents,
- drugs that are irregularly absorbed after intramuscular administration (phenytoin, digoxin, diazepam, chlordiazepoxide).
Intravenous administration[edit | edit source]
Only water-soluble substances can be administered intravenously. However, it is not necessary for them to be isotonic or to have a physiological pH, they can even be irritants. The effect of intravenously administered drugs appears quickly, usually within 2 minutes.
Increased caution is required when using substances with a low therapeutic index. Rapid application may cause a concentration wave and toxic concentrations may be reached.
Intra-arterial administration[edit | edit source]
A substance can be administered intra-arterially for which we want to achieve a high concentration in the target organ and less burden on other organs. The wave of high concentration, which is undesirable during intravenous administration, is often the goal here. Some cytostatics, contrast agents, coagulation agents for embolization of a pathological focus or, conversely, fibrinolytics for the therapy of acute arterial occlusion are administered intraarterially.
Bone marrow administration[edit | edit source]
Administering the drug into the bone marrow can ""replace intravenous administration"" in a critical situation. In children, drugs are administered into the tibia or femur, in adults into the sternum. Cannot be used in leukemia or osteomyelitis.
Intracardiac application[edit | edit source]
Direct application of the drug into the cardiac cavity is only relevant 'during resuscitation. However, it is not more convenient than intravenous administration.
Intrathecal administration[edit | edit source]
A specific feature of intrathecal administration is the need to respect the fixed volume of the space filled with cerebrospinal fluid. Substances dissolved in Ringer's solution or Tyrod's solution are administered into the subarachnoid space after collecting an adequate amount of cerebrospinal fluid. Thus, e.g. methotrexate, opiates or antibiotics are administered.
Inhalation administration[edit | edit source]
Gases, aerosols and solid particles with dimensions of 0.5-5 μm are administered by inhalation. Typically, general anesthetics and antiasthmatics are given by inhalation. The effect of inhaled substances can be local or systemic. There is usually immediate absorption and avoidance of the hepatic first-pass effect.
Transdermal administration[edit | edit source]
Mostly substances with local action (dermatology) are applied to the skin. Absorption is used in so-called transdermal therapeutic systems (nitroglycerin, scopolamine, fentanyl, nicotine. The significance is also toxicological, organophosphates are absorbed through intact skin. The rate of absorption depends on the blood supply to the given site and the type of substance (lipophilic substances are absorbed the fastest).
Links[edit | edit source]
Related Articles[edit | edit source]
References[edit | edit source]
- LINCOVÁ, Dagmar – FARGHALI, Hassan. Basic and applied pharmacology. 1. edition. Prague : Galen, Karolinum, 2002. 601 pp. ISBN 80-246-0538-4.
- LÜLLMANN, Heinz – MOHR, Klaus – WEHLING, Martin. Pharmacology and toxicology. 2nd Czech, translation 15. edition. Prague : Grada, 2004. ISBN 80-247-0836-1.