Esophageal varices 1.lf
Esophageal varices are dilated veins in the submucosa of the distal section of the esophagus. Bleeding from esophageal varices is a common complication of liver cirrhosis (in 30-60%).
Etiology and pathogenesis[edit | edit source]
The cause of varicose veins is long-lasting portal hypertension. Increased pressure leads to expansion of the portocaval junctions, specifically between the vena coronaria ventriculi (watershed of the v. portae) and venae oesophageae; vena azygos (watershed in the superior cava). There is a significant risk of bleeding from esophageal calculi when the portal pressure increases above 12 mm Hg. Large varices (> 5 mm) and thin-walled varices bleed more often.
Clinical picture and diagnosis[edit | edit source]
Varicose rupture leads to bleeding into the esophagus, which irritates the stomach and is usually manifested by bright red hematemesis. Subsequent melena is associated with the passage of blood through the digestive tract. With massive bleeding, signs of hemorrhagic shock begin to appear. Bleeding from esophageal varices is diagnosed using endoscopy.
![]() Bleeding from esophageal varices is the cause of death in half of patients with advanced liver cirrhosis.
Bleeding from esophageal varices is the cause of death in half of patients with advanced liver cirrhosis.
Therapy[edit | edit source]
In the first line, hospitalization in the ICU, provision of central venous access and administration of erymasa to replace blood loss. Subsequently, the bleeding is stopped endoscopically, by sclerotization, or ligation. Sclerotization, the operative removal of varices, must be targeted at the veins of the cardia due to the origin of the varices. Pharmacotherapy consists in inducing vasoconstriction of the splanchnic river with terlipressin - 1 mg i.v. every 4 h, possibly somatostatin (5 days).
In the case of continued bleeding, endoscopic therapy is repeated, exceptionally in case of unstoppable massive bleeding, a Sengstaken double-balloon nasogastric tube is introduced. The first balloon is fixed in the stomach, where it compresses any bleeding, and the second balloon is inflated in the esophagus, compressing the varices. Balloons are left in situ for a maximum of 24 hours, otherwise ulceration will occur. Aspiration can be a complication.
Recurrence of bleeding is very common (60-100% of patients within 2 years). β-blockers (non-selective, in sufficient doses) are used as a preventive measure, and from invasive solutions, repeated ligation/sclerotization of varices, nebp TIPS/surgical portocaval coupling operation.
TIPS[edit | edit source]
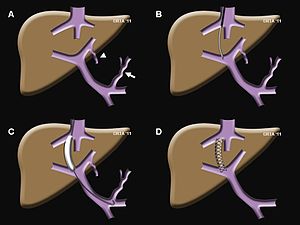
TIPS (transjugular intrahepatic portosystemic shunt) works to prevent the formation and bleeding of esophageal varices by normalizing portal hypertension. The implementation is three-step
- hepatic vein cannulation via transjugular puncture,
- puncture of the liver parenchyma and probing of the v. portae branch,
- introduction of a self-expandable stent (communication between v. portae + v. hepatica)
A complication of the procedure is the development or worsening of encephalopathy, or stenosis of the clutch.
Prognosis[edit | edit source]
Bleeding has a high lethality and frequent recurrences (prevention is essential).
Links[edit | edit source]
[edit | edit source]
References[edit | edit source]
- DÍTĚ, P., et al. Vnitřní lékařství. 2. vydání. Praha : Galén, 2007. ISBN 978-80-7262-496-6
- PETROVICKÝ, Pavel, et al. Anatomie s topografií a klinickými aplikacemi : Orgány a cévy. 1. vydání. Martin : Osveta, 2001. 560 s. sv. 2. ISBN 80-8063-046-1.
- POVÝŠIL, Ctibor. Speciální patologie. - vydání. Galén, 2007. 430 s. s. 145. ISBN 9788072624942