Granulomatous Inflammation
Specific granulomatous inflammation is a chronic inflammation, that contains special granulation tissue - epithelioid granuloma (epithelioid = resembling epithelium, granulum = grain). Epithelioid granuloma is a cluster of epithelioid macrophages (histiocytes = tissue macrophages). It is a nodular grey-white formation with a size of about 2 mm (can be seen macroscopically). The granuloma is formed by macrophages and T-lymphocytes (over time also fibroblasts).
A granuloma arises when the macrophage is unable to perform its function, i.e. to phagocytose the material. Causes of macrophage dysfunction:
- material cannot be swallowed (foreign material)
- blocking of the phagocytosis. process by some agents (e.g. TBC)
- congenital defect of phagocytosis (e.g. chronic granulomatous disease)
- long-term pathological stimulation of T-lymphocytes (in Crohn's disease)
- idiopathic (e.g. sarcoidosis)
The macrophage subsequently changes morphologically and functionally, becoming an epithelioid macrophage . It is a transformed macrophage that looks like an epithelial cell (has an epithelioid appearance). This leads to a decrease in its capacity for phagocytosis (to approximately 10%), while also decreasing the expression of some receptors. The transformed macrophage clusters with the others to join forces. Sometimes the macrophages clump together to form a syncytium , giving rise to multinucleated macrophages.
Types of multinucleated cells by disease:
- Langhans cells – in TBC and sarcoidosis (multinucleated cells with horseshoe-shaped nuclei)
- Virchow cells – in lepromatous leprosy
- Mikulicz cells - in rhinoscleroma
A granuloma may or may not have necrosis. On the periphery of the granuloma there is chronic inflammation in the form of lymphocytes (Th1) and plasma cells. It is important to note that a specific granuloma lacks vascularization - it does not contain blood vessels, it can be cold!
The formation of granulomatous inflammation[edit | edit source]
Usually, a granuloma is a reaction to something that is foreign to the body, but that macrophages cannot remove (foreign material, sutures, acid-fast mycobacteria, parasites, fungi). During the development of granulomatous inflammation, T-lymphocytes stimulate macrophages to transform into epithelioid and giant multinucleated cells (Langhans cells). The macrophage is unable to phagocytose the material and this leads to the expression of antigens on its surface. Antigens activate Th-lymphocytes, which begin to release cytokines (IL-2, TNF-gamma and interferon gamma). Cytokines stimulate the proliferation of T-lymphocytes, at the same time, they also stimulate and aggregate macrophages, which transform to form an epithelioid granuloma.
Granuloma healing[edit | edit source]
Specific granulation tissue heals by gradual fibrotization. Granulomas gradually fibrotize, hyalinize and may even calcify. Necrosis often calcifies (especially caseous). In caseous necrosis, secondary coagulation (softening and liquefaction) may also occur.
Macroscopic description[edit | edit source]
Granulomas can be microscopic (several mm) to macroscopic (several cm). The color is white-grey (does not contain vessels), the consistency is solid. Some granulomas have necrosis in the center , caseous necrosis in TBC.
Types of granuloma[edit | edit source]
There are 3 types of granuloma. We distinguish:
- immune granuloma
- arises during a hypersensitivity reaction IV. type (delayed reaction, no antibodies are formed);
- it is a cell-mediated immunopathological reaction;
- looks like a typical granuloma, there may be necrosis;
- can be blocked by immunosuppression;
- causes of granulomatous inflammation:
- tuberculosis - Mycobacterium tuberculosis
- sarcoidosis
- syphilis – Treponema pallidum
- leprosy - Mycobacterium leprae , Mycobacterium lepromatosis
- foreign body granuloma (non-immune)
- arises in material without antigenic properties;
- it arises, for example, around stitches, parasites or foreign bodies;
- it arises when the macrophage is unable to phagocytose foreign material;
- often it is not a fully developed granuloma, but just a cluster of multinucleated cells (nuclei in the center);
- it cannot be blocked by immunosuppression;
- granuloma of unknown cause
- for example in sarcoidosis or Crohn's disease
Types of granulomas[edit | edit source]
Types of granulomas:
- circumscribed granulomas without necrosis - for example, in sarcoidosis or Crohn's disease;
- a granuloma that has caseous necrosis in the center and palisade macrophages around it - eg TB, syphilis;
- granuloma, which has a small abscess with pus in the center, contains neutrophils and granulomas on the periphery;
- it is called so-called granulomatous purulent inflammation (combination of specific and non-specific inflammation);
- occurs mainly in bacterial infections and mycoses (e.g. brucellosis, cat scratch disease);
- a granuloma that has fibrinoid necrosis in the center - for example, in rheumatic fever.
Cells of granulomatous inflammation[edit | edit source]
Epithelioid cells[edit | edit source]
- they arise from the transformation of normal macrophages and monocytes that have migrated to the site of damage;
- they rarely contain phagocytosed material;
- have reduced phagocytic function by 90% compared to macrophages;
- they lack expression of Fc and C5a receptors;
- they have a significant secretory function, in the electron microscope we therefore see a well-developed granular endoplasmic reticulum and the Golgi apparatus;
- in some diseases, notably sarcoidosis, these cells produce angiotensin-converting enzyme and also activate cholecalciferol, which induces hypercalcemia.
Giant multinucleated cells of the Langhans type[edit | edit source]
- they arise from the fusion of the cytoplasm of macrophages, therefore they have up to several tens of nuclei;
- the nuclei tend to be arranged on the periphery of the cytoplasm in a circle, or around the entire perimeter of the cells;
- they do not differ structurally or functionally from epithelioid cells;
- if they are cells from foreign bodies, then we will demonstrate indigestible material in their cytoplasm.
Examples of diseases[edit | edit source]
- Tuberculosis ( Mycobacterium tuberculosis )
- Syphilis ( Treponema pallidum )
- Leprosy ( Mycobacterium leprae )
- Reaction to foreign bodies (stitches)
- Silicosis
- Bilharziasis
- Sarcoidosis
- Crohn's disease
Granulomatous versus specific inflammation[edit | edit source]
Granulomatous and specific are actually the same thing. It is granulomatous according to the macro appearance (makes granules). Specific means that we know by the macro appearance that the inflammation is caused by something that is known to cause that type of inflammation. The choice of etiological agent is much narrower than in non-specific inflammation, where the same macro appearance (eg, suppuration) will trigger a "million" species of bacteria. Non-specific granulation tissue is formed within the healing (proliferative) phase of non-specific inflammation, eventually a scar is formed and this tissue is highly vascularized.
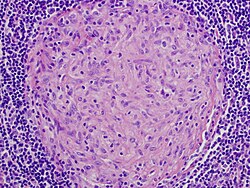
Non-necrosis granulomas in the airways in sarcoidosis
Granuloma without necrosis in a patient with sarcoidosis
Centrally necrotizing granuloma in a patient with tuberculosis . Large Langhans cells can be seen at the periphery of the granuloma¨.
Links[edit | edit source]
Related Articles[edit | edit source]
References[edit | edit source]
- STŘÍTESKÝ, Jan. Pathology. 1. edition. 2001. ISBN 80-86297-06-3.
Links[edit | edit source]
- ŠTEFÁNEK, George. Granulomatous inflammations [online]. [cit. 2017-06-26]. <https://www.stefajir.cz/?q=granulomatozni-zanety>.