Hemorrhagic stroke / PGS / diagnostics
Template:PGS
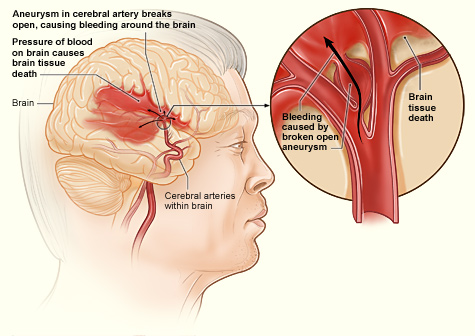
Hemorrhagic strokes are divided into two large, partially co-occurring groups: intracerebral haemorrhage and subarachnoid or intraventricular haemorrhage.
Definition[edit | edit source]
Bleeding into brain tissue, possibly with associated ventricular bleeding or subarachnoid haemorrhage .
Clinical picture[edit | edit source]
Same as ischemic stroke or finding very rapidly progressing to loss of consciousness or early onset of epileptic manifestations. Clear resolution is only possible on the basis of an imaging examination.
Causes[edit | edit source]
| The most common causes |
|---|
|
Classification[edit | edit source]
By location:
typical central bleeding - "hypertonic" intracerebral bleeding based on small vessel disease complex;
atypical lobar hemorrhage - intracerebral hemorrhage based on the above causes (Tab.4).
Examination procedure and treatment[edit | edit source]
The same algorithm as in any acute neurological patient (Chapter 2) or in a patient with impaired consciousness (Chapter 3), possibly as in patients with intracranial hypertension syndrome (Chapter?), With emphasis on early CT of the brain and subsequent transport to the ICU (intensive care unit ). care) regardless of the type of bleeding and any good clinical condition of the patient.
In the case of atypical hemorrhage, it is necessary to consult the neurosurgical workplace with regard to further investigation of the causes and consideration of a possible neurosurgical intervention (decompression, ventricular drainage). In younger patients without risk factors, it is necessary (even with a delay) to exclude the source of bleeding at any location ( MR brain, MR angio, DSA, CT angio).
Treatment of spontaneous intracerebral haemorrhage and prevention of its progression takes place only in the relevant ICU.
- blood pressure control (correction of systolic blood pressure above 180 in hypertensive patients, optimally up to 160)
- correction of hypocoagulation disorder (application of vitamin K, frozen plasma, recombinant activated plasma factor VII).
- reduction of intracranial pressure - antiedematous therapy - mannitol
- analgesia / relaxation, artificial lung ventilation - permissive hypocapnia
- barbiturate coma
- hypothermia
- elimination of intracranial pressure fluctuations - laxatives, antitussives
- consideration of an indication for decompression craniectomy


