Heparin
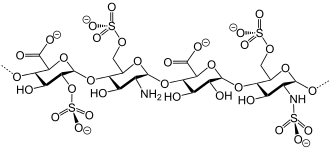
Heparin is a heterogeneous mixture of sulfonated polysaccharides (glycosaminoglycan) with anticoagulant effects, which is contained mainly in granules of basophilic granulocytes and mast cells. It is normally present in the body (produced by mast cells, it occurs mainly in the liver, lungs and intestine). Classical heparin - i.e. unfractionated heparin and its derivatives - low molecular weight heparins and pentasaccharides are used therapeutically. Heparin is prepared by extraction from the intestinal mucosa of pigs and the lungs of cattle.
Main effects[edit | edit source]
Heparin acts as a catalytic cofactor for antithrombin. Antithrombin III (AT III) is α 2 -globulin synthesized in the liver. It is a natural inhibitor of thrombin (F IIa) and other serum proteases (F IXa, Xa, XIa), with which it forms an irreversible complex.
Other effects[edit | edit source]
Heparin releases lipoprotein lipase from the endothelium, which conditions its antilipidemic effect. It further reduces platelet adhesion to the endothelium, reduces platelet-derived growth factor releasing, and has a mild antihistaminic effect. Its anticoagulant effect can also be used in vitro.
Method of administration and pharmacokinetics[edit | edit source]
Heparin is effective only after intravenous (immediate effect) or subcutaneous (effect after about 2 hours ) administration. Intramuscular administration is not recommended due to the risk of haematomas at the injection site.
For full anticoagulation, a dose of 0.01 ml/kg of patient weight is administered twice daily to either low molecular weight heparin (eg. Fraxiparine, Clexane) s.c. or unfractionated heparin i.v. using a perfuser.
Immediately after administration, heparin binds to vascular endothelial receptors. Heparin does not cross the placenta or into breast milk, so it can be used during pregnancy.
Indication[edit | edit source]
Heparin is used for anticoagulant and antithrombotic purposes. The main use is in the following indications:
- venous thromboembolism - in therapy to prevent the growth of an already formed thrombus,
- disseminated intravascular coagulation - (DIC)
- unstable angina pectoris
- cerebrovascular thromboembolism
Monitoring of heparin treatment[edit | edit source]
Today, APTT is used for monitoring heparin treatment. Extension of the APTT (depending on the type of reagent used) is recommended 2-4 times. Since the effect of heparin depends on the presence of AT III, it is advisable to monitor its level during prolonged treatment.
Antidote[edit | edit source]
Protamine sulfate, a peptide obtained from salmon sperm, can be used as an antidote to block the anticoagulant effect after open-heart surgery, after dialysis, in heparinized patients before acute surgery and in case of excessive or life-threatening bleeding. This basic sulfate binds to heparin to form an inert complex. The dose required to bind 1 mg heparin (100 IU) is 1 to 1.5 mg. Protamine sulphate is given as a slow infusion to prevent adverse reactions (thrombosis, hypotension, dyspnoea, anaphylactic reaction).
Contraindications to heparin[edit | edit source]
Absolute- represent conditions with a high risk of severe bleeding, such as acute gastrointestinal bleeding, intracranial bleeding, uncontrolled hypertension, haemorrhagic diathesis (haemophilia, severe thrombocytopenia), heparin-induced thrombocytopenia.
Relative- represent conditions with increased readiness for bleeding, where the risk of possible bleeding must be weighed against the severity of a thrombotic condition, such as large vessel thrombosis, a condition immediately after vascular reconstruction, etc.
Adverse effects of heparin therapy[edit | edit source]
Bleeding is a major side effect of heparin therapy. It is observed more frequently in patients treated with therapeutic doses than in prophylactic doses. Major bleeding occurs in 1 to 10% of treated patients, fatal bleeding occurred in 3 of 647 treated patients according to one study.
Heparin may also induce thrombocytopenia(antibody production to platelet factor 4). Osteoporosis may occur with long-term administration.
Links[edit | edit source]
Related Articles[edit | edit source]
External links[edit | edit source]
References[edit | edit source]
- LINCOVÁ, Dagmar – FARGHALI, Hassan. Základní a aplikovaná farmakologie. 2.. edition. Praha : Galén, 2007. pp. 672. ISBN 978-80-7262-373-0.
- ŠVÍGLEROVÁ, Jitka. Wayback machine [online]. [cit. 5.12.2021]. <https://web.archive.org/web/20160416170033/http://wiki.lfp-studium.cz/index.php/Heparin>.
- AHMED, I. Heparin induced thrombocytopenia: diagnosis and management update. Postgraduate Medical Journal [online]. 2007, y. 2007, p. 582, Available from <https://pmj.bmj.com/content/83/983/575.full>. ISSN 1469-0756.
Used literature[edit | edit source]
- LINCOVÁ, Dagmar – FARGHALI, Hassan. Základní a aplikovaná farmakologie. 2.. edition. Praha : Galén, 2007. pp. 672. ISBN 978-80-7262-373-0.