Mycotic diseases in the newborn age
From WikiLectures
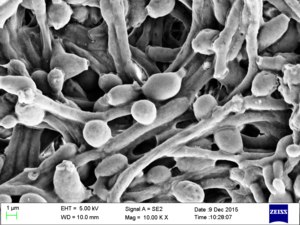
Mycotic diseases of newborns are most often caused by Candida species. The most common manifestations include skin and mucosal infections. Systemic fungal diseases are relatively less common in newborns, bacteria and viruses are much more common causes of infections. Disseminated fungal infections are serious and often fatal.[1]
The causative agents of mycotic diseases are classified as fungi, they are found freely in nature, they tend to have low pathogenicity and often colonize mucous membranes without symptoms.[1]
Risk Factors[edit | edit source]
- prematurity and very low birth weight (immature immune system, insufficiently developed skin epithelium and mucosal barriers, need for a number of invasive procedures - central venous catheter, endotracheal intubation, etc.);
- long-term administration of broad-spectrum antibiotics, administration of corticosteroids;
- long-term total parenteral nutrition, long-term administration of fat emulsions and infusion solutions with a high concentration of glucose (20-40%);
- advertising of central venous catheters;
- cervical cerclage.[1]
Candida infections[edit | edit source]
- Candida albicans (60 - 75%), C. parapsilosis (20 - 30%), C. tropicalis, C. lusitaniae, C. glabrata, C. krusei;
- sepsis, less often meningitis, endocarditis, kidney, spleen and liver abscesses, endophthalmitis, skin infections, urinary infections, osteomyelitis;
- candidemia can be primary or secondary (e.g. in primary urinary tract infection, etc.);
- vertical transmission (from the mother during childbirth or breastfeeding) and horizontal (from medical personnel or contaminated objects);
- Candida sp. generally colonizes the skin, digestive tract, genitalia, intertriginous areas; colonization usually precedes invasive infection, newborns are usually infected with the same strain they were first colonized with;[2]
- == Candida infections ==
- Candida albicans (60 - 75%), C. parapsilosis (20 - 30%), C. tropicalis, C. lusitaniae, C. glabrata, C. krusei;
- sepsis, less often meningitis, endocarditis, kidney, spleen and liver abscesses, endophthalmitis, skin infections, urinary infections, osteomyelitis;
- candidemia can be primary or secondary (e.g. in primary urinary tract infection, etc.);
- vertical transmission (from the mother during childbirth or breastfeeding) and horizontal (from medical personnel or contaminated objects);
- Candida sp. generally colonizes the skin, digestive tract, genitalia, intertriginous areas; colonization usually precedes invasive infection, newborns are usually infected with the same strain they were first colonized with;[3]
Acute pseudomembranous candidiasis (thrush, thrush) - non-invasive mucocutaneous candidiasis[edit | edit source]
- whitish, gooey, coagulated milk-like coatings on the buccal mucosa, tongue mucosa and gums; after wiping, the base is red, inflamed and may bleed easily;
- on a larger scale, pain or even eating disorders;
- can also spread to the oropharynx; often associated with candidal dermatitis in the perianal and perigenital area - erythematous vesiculo-pustular efflorescence with desquamation and oozing;
- T-lymphocytes play an important role in mucosal immunity against candida;
- pseudomembranes are formed by epithelial cells, leukocytes and candida;
- treatment: local skin or oral preparations of nystatin (oral suspension 100,000 IU/ml, 0.5 ml on each side of the mouth 4 times a day between meals, 5-10 days + decolonization/sterilization of teats, teats, etc.)[4], miconazole, clotrimazole, econazole, natamycin and others; in the case of extensive thrush with simultaneous perianal skin infection, general administration of oral antifungals - fluconazole (3 mg/kg, 1x daily p.o. for 7 days) is appropriate [4] or ketoconazole.[1]
Congenital generalized cutaneous candidiasis[edit | edit source]
- maculopapular efflorescence on the skin of the chest and limbs, which quickly turns into pustules that burst; their base is slightly reddened and sharply demarcated;
- consequence of ascending intrauterine infection;
- often does not require treatment, or topical antifungals can be used.[1]
Systemic (generalized) candidiasis[edit | edit source]
- CNS, kidney and lung involvement predominates in newborns;
- the clinical picture is non-specific, similar to bacterial sepsis - thermolability, icterus, loss of appetite, abdominal distension, vomiting, respiratory difficulties, circulatory disorders, hypotension, shock, apathy, lethargy, irritability, maculopapular rash, hypo- or hyperglycemia;
- treatment: parenteral administration of antifungals - fluconazole (12 mg/kg i.v. every 24 h)[4], amphotericin B (1 mg/kg i.v. every 24 h)[4]; at least 21 days for sepsis and 28 days for meningitis.[1]
Unusual fungal infections[edit | edit source]
Aspergillosis[edit | edit source]
- Aspergillus fumigatus, A. flavus, A. niger;
- very high mortality even with antifungal treatment;
- the primary infection usually affects the skin (erythema -> hemorrhagic bullae -> ulceration) or the respiratory tract (pneumonia when inhaling spores) with the risk of rapid systemic dissemination (respiratory failure, liver failure, convulsions, skin lesions, thrombosis, infarctions, necrosis);
- diagnosis: microscopic examination, culture, PCR of serum or cerebrospinal fluid.
Zygomycosis (mucormycosis)[edit | edit source]
- Rhizopus, Mucor, Absidia;
- primary infection usually affects the skin or digestive tract (necrotizing enterocolitis without radiological changes; high mortality); vascular thrombosis, tissue necrosis;
- diagnosis: histopathological; cultivation often unsuccessful;
- treatment: debridement, surgical resection; amphotericin B.
Malassezia[edit | edit source]
- Malassezia furfur, M. pachydermatis, M. globus, M. sympodialis;
- colonizes the skin, rarely the respiratory tract;
- with the exception of M. pachydermatis, they need exogenous long-chain fatty acids for their growth.
Dermatophytosis[edit | edit source]
- Epidermophyton, Trichophyton, Microsporum;
- tinea faciei, tinea capitis, tinea corporis, extensive skin lesions;
- treatment: topical antifungals.
Treatment[edit | edit source]
- neonatal invasive fungal infection: amphotericin B, ev. in combination with fluconazole or flucytosine in CNS infection;
- amphotericin B - broad-spectrum antifungal (Candida sp., Aspergillus sp., etc.); parenteral form of administration only; disrupts the synthesis of the fungal wall; worse permeability to the CNS; it is usually given for at least 14 days after sterilization of the infection site; potentially nephrotoxic - rarely in newborns;
- fluconazole - triazole; prevents the formation of ergosterol, the main component of the cell membrane of mushrooms; intravenous or oral administration; good penetration into the CNS;
- flucytosine - cytosine analog; disrupts DNA synthesis; narrow spectrum - acts against candida and cryptococcal infections; risk of rapid development of resistance in monotherapy; excellent penetration into the CNS, synergistic effect with amphotericin B; enteral administration only.[5]
Video[edit | edit source]
Links[edit | edit source]
Related articles[edit | edit source]
- Infections in the neonatal period • Antibiotics (neonatology)
- Mycoses • Candidosis • Invasive fungal infections • Antimycotics
References[edit | edit source]
- ↑ a b c d e f JANOTA, Jan – STRAŇÁK, Zbyněk. Neonatologie. 1. edition. Mladá fronta, 2013. pp. 270-274. ISBN 978-80-204-2994-0.
- ↑ PAMMI, M. Epidemiology and risk factors for Candida infection in neonates [online]. UpToDate, ©2019. [cit. 2020-09-05]. <https://www.uptodate.com/contents/epidemiology-and-risk-factors-for-candida-infection-in-neonates>.
- ↑ PAMMI, M. Prevention of Candida infection in neonates [online]. UpToDate, ©2019. The last revision 2020-04, [cit. 2020-09-05]. <->.
- ↑ a b c d PAMMI, M. Treatment of Candida infection in neonates [online]. UpToDate, ©2018. The last revision 2020-04, [cit. 2020-09-06]. <https://www.uptodate.com/contents/treatment-of-candida-infection-in-neonates>.
- ↑ PAMMI, M. Unusual fungal infections in the neonate [online]. UpToDate, ©2018. The last revision 2020-04, [cit. 2020-09-05]. <https://www.uptodate.com/contents/unusual-fungal-infections-in-the-neonate>.