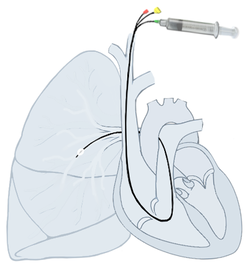
Right heart catheterization
To monitor the pressure in the pulmonary artery, a Swan-Ganz catheter is used. It is introduced through the right heart into the pulmonary artery and wedged into one of its branches by an inflated balloon. Modern catheters are able to measure more parameters ,and by gradual introduction it is possible to measure central venous pressure, and pressure in the right atrium, right ventricle, and in the lungs. Indications have been limited recently due to the possibility of detecting many cardiovascular parameters using other methods, especially ultrasonography. The main purpose of this catheter is to measure the wedge pressure, because it is not measurable in any other way. Right heart catheterization can also be used for differential diagnosis and definitive confirmation of the diagnosis of pulmonary hypertension.
Parameters that are directly measurable:
- pressure in the pulmonary artery, central venous pressure
- wedge pressure
- cardiac output
- saturation of mixed venous blood
- central body temperature
Other circulation parameters that can be calculated from the measured parameters:
- systemic and pulmonary vascular resistance
- heart rate volume
- oxygen consumption and supply
- left and right ventricular stroke work index
Pulmonary hypertension[edit | edit source]
Catheterization makes it possible to measure pressure in the vessels of the lungs and compare it with the wedge pressure, which will make it possible to distinguish between precapillary and postcapillary causes of pulmonary hypertension. By definition, pulmonary hypertension is considered to be a mean pulmonary artery pressure > 25 mm Hg.
Wedge pressure[edit | edit source]
Wedge Pressure (PCWP, Pulmonary Capillary Wedge Pressure) is the pressure in the final branch of the lung after sealing with a balloon. After stopping the flow from the pulmonary artery branch with the balloon, the pressures equalize and wedge pressure should be equal to the pressure in the left atrium, revealing some of the functions of the left heart. The physiologic range is 2-12 mmHg. [1] The pressure fluctuates depending on the heart cycle, similar to a phlebogram. The pressure level is usually used to assess ventricular filling (preload) and hydrostatic pressure in the pulmonary capillaries.
Elevated PCWP is associated with conditions that increase left ventricular end-diastolic pressure such as left-sided systolic and diastolic heart failure, mitral and aortic valve defects, hypervolemia, right-to-left shunts, cardiac tamponade, and hypertrophic, constrictive or restrictive cardiomyopathy.
Decreased PCWP is present in hypovolemia, pulmonary veno-occlusive disease, or massive pulmonary embolism.
Other measured parameters[edit | edit source]
Today, these measured parameters can usually be determined using ultrasonography or other non-invasive methods.
Measurement of minute cardiac output (CO)[edit | edit source]
- This is the volume of blood expelled by the heart within 1 minute.
- Physiologic range: 4–8 l/min
- Cardiac index: 2.5–4.5 L/min/m 2 of body surface area
- It can be measured in several ways:
Thermodilution[edit | edit source]
- At the end of the inserted floating Swan-Ganz catheter is a thermistor.
- 10 mL of physiologic saline is injected through the outer end of the catheter. This solution is at room temperature (approximately 18-22 °C).
- The thermistor at the inserted end shows a curve that is the result of a change in the temperature of the surrounding blood over time.
- The smaller the cardiac output, the more slowly the infused solution flows around the thermistor and the smaller the temperature difference is as represented by a larger area under the curve.
Dilution method with dye indicator[edit | edit source]
- Fluid volume within the circulatory system is determined using the concentration of an indicator (in a peripheral artery). A known amount (concentration and volume) of this indicator has been dissolved in a fluid administered to the patient.
Fick's principle[edit | edit source]
- The volume of blood flowing into the lungs per minute = cardiac output
- This value is given by: (patient's oxygen consumption/min) / (oxygen content in arterial blood - oxygen content in mixed venous blood)
Measurement of vascular resistance[edit | edit source]
Vascular resistance is can be measured using Ohm's law: vascular resistance is equal to the ratio of the pressure gradient to the blood flow ().
Pulmonary vascular resistance (PVR)[edit | edit source]
- Physiologic range: 20–130 dynes/s/cm-5,
- ,
- (TPG: transpulmonary pressure gradient; CO: cardiac output; PAP: mean pulmonary arterial pressure; LAP: mean left atrial pressure or wedge pressure)
- This parameter is determined before cardiac surgery (congenital heart defects, heart transplants).
Peripheral (systemic) vascular resistance (SVR)[edit | edit source]
- Physiologic range: 700–1600 dynes/s/cm-5,
- ,
- (AOP: mean aortic pressure; RAP: mean right atrial pressure; CO: cardiac output)
- This parameter is significant in monitoring heart failure (reduction may lead to improvement).
Links[edit | edit source]
Related Articles[edit | edit source]
Sources[edit | edit source]
- DÍTĚ, P., et al. Vnitřní lékařství. 2. vydání. Praha: Galén, 2007. ISBN 978-80-7262-496-6.
- SILVESTRY, Frank E. Pulmonary artery catheterization: Interpretation of hemodynamic values and waveforms in adults [online]. UpToDate, Poslední revize 2020-01-14, [cit. 2020-05-13]. <https://www.uptodate.com/contents/pulmonary-artery-catheterization-interpretation-of-hemodynamic-values-and-waveforms-in-adults>.
References[edit | edit source]
- ↑ ŠEVČÍK, Pavel, et al. Intensive care medicine. 3rd edition. Galén, 2014. 1195 pp. 157–161. ISBN 9788074920660.