Sickle Cell Anemia
Definition[edit | edit source]
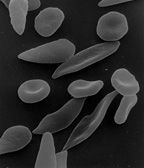
Sickle cell anemia is a hereditary disorder of autosomal recessive inheritance that is characterized by sickle-shaped red blood cells. It is the most common type of hemoglobinopathy and is the result of a mutation in the β-globin chain gene that results in creating sickle hemoglobin (HbS) instead of the normal adult hemoglobin (HbA).
Sickle cell anemia:
Sickle Cell Anemia 2:
Etiology, Incidence[edit | edit source]
- The mutation responsible for this abnormal HbS, is a single amino acid substitution in the globin chain. Specifically, there is a substitution of valine for glutamic acid at the sixth position of the β-globin chain. Since it is a recessive gene, heterozygotes are carriers and have about half of their HbA replaced by HbS, whereas homozygotes have exclusively HbS.
- Although sickle cell anemia has a low incidence in Europe, it is quite frequent for regions such as Africa and Middle-East. Particularly, about 75% of sickle cell anemia cases occur in Africa.
Pathogenesis[edit | edit source]
- When HbS is deoxygenated (e.g. in venous capillaries) it undergoes polymerization in a process also called gelation or crystallization. The result of this polymerization, are long polymers that deform the structure of red blood cell. It acquires the characteristic sickle shape.
- If this deoxygenation continues, it eventually causes damage on the cell membrane and dehydration of red blood cells, making them irreversible sickled. Since these sickle-shaped red blood cells are rigid, abnormal and dysfunctional, they are removed from the body by macrophages, leading to extravascular hemolytic anemia
- Red blood cells are more fragile, therefore they have a shorter life span of about 20 days (instead of the normal 120 days life span).
- Another major consequence is that these membrane changes increase the adhesiveness of the sickle cells, which can cause throughout the body microvascular obstructions, leading to local ischemia, tissue damage and pain crises.
- The sickling of red blood cells depends on many changing factors:
- The amount of hemoglobin present in red cells excluding HbS. As mentioned above, in heterozygotes half of their hemoglobin is HbS.Therefore, the remaining HbA can influence the rate of polymerization and sickling occurs little or not at all.
- The amount of HbS in red cells influences the tendency of HbS to form polymers. For example, dehydration of red cells increases the concentration of HbS and promotes sickling.
- The time that red cells are exposed to low concentrations of oxygen. Red blood cells passing through microvascular beds where blood flow is diminished, are exposed to lower oxygen tension and sickling is easier to happen. This usually happens in bone marrow and spleen. In addition, inflamed tissues have also a decreased blood flow so sickling is more likely to happen.
Morphology[edit | edit source]
- Extravascular hemolytic anemia, which can be severe.
- The increased destruction of this abnormal red cells result in the release of heme, which is converted into bilirubin. Increase of bilirubin concentration in blood leads to jaundice.
- In addition to bilirubin, during the destruction of red blood cells, iron is also released in circulation leading to hemosiderosis.
- The microvascular occlusions caused by sickle cells lead to tissue ischemia. As a result, infarction and thrombosis are more likely to occur and can affect any organ such as liver, kidney,brain.
- In blood smear there are elongated sickled red cells, easily identified.
- The anemia can cause fatty changes in liver, heart and tubules of the kidneys.
- The low amounts of normal hemoglobin in the blood is compensated by hematopoiesis outside of the medulla in bone marrow (i.e. extramedullary hematopoiesis).
- In children, there is some degree of splenomegaly, which is caused by high amounts of sickle cells in red pulp of spleen destined to be destroyed. On the other hand, this can lead slowly to hypoxic tissue damage of spleen. As a result, it reduces the size of the spleen in a process called autosplenectomy.
Sickle Cell Anemia and Malaria[edit | edit source]
Malaria is an infectious disease caused by the Plasmodium parasites, that infect and multiply within the red blood cells. As mentioned above, homozygotes with the mutated gene for HbS have exclusively HbS and all their red blood cells acquire the characteristic sickle shape. Heterozygotes have slightly different shaped red blood cells, that is neither the normal concave shape or the abnormal sickle shape. Therefore, heterozygotes when exposed to the Plasmodium parasites, it is more difficult to be infected since the parasites will not be able to enter their red blood cells. At the end, heterozygotes are protected from malaria and are only carriers of the mutated gene for sickle cell anemia and do not exhibit any signs of the disease. This was observed in some regions in Africa, where malaria is an epidemic and sickle cell anemia has high incidence.
Links[edit | edit source]
Related articles[edit | edit source]
Bibliography[edit | edit source]
VINAY, Kumar. Basic Pathology. 8. edition. 2007. ISBN 978-1-4160-2973-1.