Skin sarcoidosis
Sarcoidosis is a multisystem disease of unknown cause. It most often affects young people and middle-aged people, more women. It is often manifested by bilateral hilar adenopathy, pulmonary infiltrates, ocular and skin lesions. The liver, spleen, lymph nodes, salivary glands, heart, nervous system, muscles, bones and other organs can also be affected. Forms of skin involvement are divided into non-specific and specific according to the presence or absence of non-caseifying granulomas at biopsy.
Epidemiology[edit | edit source]
The disease occurs worldwide. About 25 % of patients are affected. Specific disabilities occur in 10.5 % of cases. Lupus pernio occurs more often in blacks and Indians, especially in older women.
Symptoms[edit | edit source]
The most common form of a non-specific skin lesion is erythema nodosum (28.2% in our country). It is a symptom of acute sarcoidosis and often occurs in Europeans. It usually disappears within 6-8 weeks. Erythema nodosum is not pathognomonic for sarcoidosis in relation to infections, neoplasms, vasculitis and drug reactions. Erythema nodosum as part of Löfgren's syndrome, together with fever and bilateral hilar lymphadenopathy (BHL), is so specific to sarcoidosis that it does not require histological evidence of non-caseifying granulomas in the event of spontaneous and rapid remission of symptoms.
The most common specific lesion is lupus pernio. Represents chronic sarcoidosis. It manifests as indurated areas, painless, itchy, without ulceration, associated with the decolorization of the nose, lips, eyelids and scars. It is often associated with bone cysts, nasal mucosa and lung fibrosis. Spontaneous remissions are rare.
Other specific skin manifestations may include maculopapular eruptions, subcutaneous nodules, infiltration of old scars, and skin plaques.
Treatment[edit | edit source]
For erythema nodosum, nonsteroidal antirheumatic drugs are usually sufficient. For small sarcoid papules and plaques, monthly intrapapular injection of triamcinolone or weekly topical treatment with corticoids and hydrocolloids is possible. Larger or defiguring lesions require systemic treatment.
- an alternative regimen of 30 mg Prednisone
- weekly pulse regimen with Methotrexate
- hydrochloroquine
New infliximab, allopurinol, thalidomide.
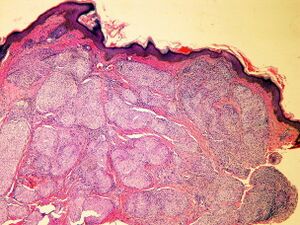
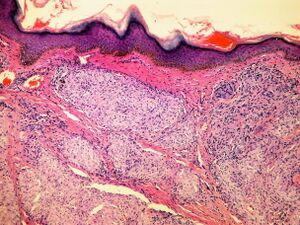
Histology[edit | edit source]
Sharply demarcated circular non-caseifying granulomas. Composed of epithelioid macrophages (histiocytes), surrounded by a negligible lymphocyte infiltrate. They are therefore referred to as "naked".
References[edit | edit source]
Related articles[edit | edit source]
Sources[edit | edit source]
- ANTON, Jan. Materials for the lecture "Sarcoidosis".
References[edit | edit source]
HUNNINGHAKE, G W – COSTABEL, U – ANDO, M. , et al. ATS/ERS/WASOG statement on sarcoidosis. American Thoracic Society/European Respiratory Society/World Association of Sarcoidosis and other Granulomatous Disorders. Sarcoidosis Vasc Diffuse Lung Dis [online]. 1999, y. 2, p. 149-73, Available from <https://www.ncbi.nlm.nih.gov/pubmed/10560120>. ISSN 1124-0490.
Used literatures[edit | edit source]
- ŠTORK, Jiří, et al. Dermatovenerologie. 1. edition. Praha : Galén, Karolinum, 2008. 502 pp. ISBN 978-80-7262-371-6.