Sarcoidosis (pathology)
Sarcoidosis:
Sarcoidosis is a multisystem disease of unknown cause. It most often affects young and middle-aged people, more women. The diagnosis is established if the radiological findings are supported by histological evidence of non-caseating epithelioid cell granulomas. Granulomas of known causes and local sarcoid reactions must be excluded.
Characteristics[edit | edit source]
Sarcoidosis is a systemic granulomatous disease, that predominantly affects young women. It usually begins with the involvement of the nodes of the chest cavity (bilateral hilar syndrome), then affects the lungs, spleen, liver, skin, bones, uveal tract, parotid gland (parotid sarcoid associated with involvement of the uvea is referred to as Heerfordt syndrome), more rarely the myocardium, kidneys and other organs.
Clinically, it can be manifested by breathing difficulties, the development of cor pulmonale, lymphadenopathy suspected of cancer, subcutaneous nodules, red raised areas on the skin, xerostomia and xerophthalmia, etc. It differs from tuberculosis in its slow development rare involvement of the serous membranes and adrenal glands, and the tuberculin reaction is negative.
Etiology[edit | edit source]
The etiology is unknown, genetic factors, infectious agents, immunopathological processes are considered (type IV immunopathological reaction to low-virulence mycobacteria and their products, or abnormal reactions to various antigens and allergens). There appears to be no specific agent or single discrete immunological defect causing sarcoidosis.
Granulomatous reaction represents an "immunological fallback" in individuals who are unable to clear the immunological agent in a more efficient manner. The development of sarcoidosis is thus explained by a specific interaction between one or several exposures and one or several types of immune response.
- Possible triggers:
- Bacteria: M. TBC, atypical mycobacterium, Propionibacterium acnes, Rickettsia, Borrelia, Mycoplasma.
- Viruses: EBV.
- Inorganic substances: Al, Zr, mineral fibers, Si, silicon, clay, talc.
- Organic substances: pine pollen, starch.
Pathogenesis[edit | edit source]
Macrophages, apparently due to the interaction of the antigen with IFN-gamma, have an increased expression of HLA II molecules and present the expected antigen to CD4 cells of the T h 1 type and through the production of IL-12 cause further accumulation of CD4 cells and their differentiation into the T h 1 type with subsequent production of IFN-gamma . These activated T-cells release IL-2 and chemotactic factors causing the accumulation of monocytes and macrophages at the site of disease activity and the expansion of various T-cell clones. IFN-gamma further activates macrophages and transforms them into epitheloid and multinucleated giant cells that form the basis of the granuloma and produce ACE. Macrophages produce TNF-alpha, which is a key cytokine for granuloma integrity. Lymphocytes CD4, CD8 and a smaller amount of B-lymphocytes then form a rim around the granuloma.
Already in the early stage of granuloma formation, in some individuals, probably due to the increased production of macrophage fibrogenic cytokines (TGF-beta, PDGF, IGF-I) or because the antigen is presented by a different HLA class, cytokine production shifts to the Th2 (IL-4, IL-6, IL-15). This response does not lead to elimination of the pathogen and results in continuous granuloma formation with chronic disease. For unclear reasons, in some cases this cluster of cells begins to be enveloped by a strip of fibroblasts, mast cells. collagen fibers and proteoglycans. This fibrotic response can cause substantial, often irreversible, organ destruction and physiological dysfunction.
Histological differential diagnosis[edit | edit source]
- TBC, atypical mycobacteriosis, brucellosis, toxoplasmosis, granulomatous histiocytic necrotizing lymphadenitis, cat scratch disease.
- Sarcoid reaction in cancer, Hodgkin disease, non-hodgkin lymphoma.
- GLUS syndrom (granulomatous lesions of unknown significance).
Epithelioid granuloma[edit | edit source]
Epithelioid granuloma is a compact mass formed by lymphocytes and highly differentiated mononuclear phagocytes (epithelioid and Langhans cells). The central area of the granuloma is formed mainly by CD4 lymphocytes, while CD8 lymphocytes are present in the peripheral zone. Unlike tuberculosis there is no central caseification (but there may be coagulation necrosis with pyknotic nuclei) or calcification, and the lymphoplasmacytic border is also less marked. Several types of inclusions are found in Langhans cells (but not specific to sarcoidosis):
- asteroid inclusions – star-shaped, stains on elastic (orcein, resorcin-fuchsin), eosinophilic in HE
- Schaumann inclusions – layered, round in shape, contain Ca and Fe, stain blue in HE
- calcite inclusions – crystalline, do not stain, are refractive and bend the plane of polarized light
The nodules may dissolve, or their healing begins with fibrosis at the periphery. The end result is a trabecular or more or less compact hyaline scar. The healing of sarcoidosis in the lungs leads to the formation of scars with the disappearance of elastic, in the bones there is resorption of bone beams in the granuloma deposits, and even cirrhotic remodeling can occur in the liver.
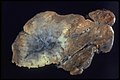
Macroscopy[edit | edit source]
Organs affected by sarcoidosis enlarge, nodules are visible on the surface, later marked fibrotization to hyalinization.
- Macroscopic images – lungs
- Microscopic images – lungs
- Microscopic images – granuloma development
Links[edit | edit source]
Related articles[edit | edit source]
- Extrapulmonary Sarcoidosis
- Sarcoidosis/Lymphatic system
- Sarcoidosis/Heart
- Sarcoidosis/Liver
- Sarcoidosis/Eyes
- Sarcoidosis/Skin
- Sarcoidosis/Musculoskeletal
- Hypercalcemia in sarcoidosis
- Sarcoidosis/Blood
- Sarcoidosis (internal)
Source[edit | edit source]
- PASTOR, Jan. Langenbeck's medical web page [online]. ©2005. [cit. 8.10.2011]. <https://langenbeck.webs.com/>.
ANTON, Jan. Materials for the lecture "Sarcoidosis". (Shortened, edited)