Structure Vessels
Vessels[edit | edit source]
Blood vessels are part of the lymphatic and cardiovascular systems. Through the cardiovascular system, oxygen and nutrients are distributed in the body to the tissues and waste products of metabolism to the excretory organs. Furthermore, the transport of hormones to target organs is mediated. The lymphatic vascular system is used to return fluid from the interstitial spaces to the blood circulation. These systems thus contribute to the integration of the function of the whole organism.
The blood vessels are divided into blood and lymphatic vessels.
For blood vessels, we further distinguish between arteries, veins and capillaries.
General structure of blood vessels[edit | edit source]
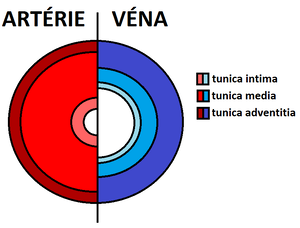
Blood vessels are composed of three basic structures: tunica intima, tunica media and tunica adventitia.
Tunica intima[edit | edit source]
- It consists of a layer of endothelial cells overlying the basal lamina and a layer of subendothelial cells.
Endothelial cells[edit | edit source]
- Polygonal, flat;
- Stretched in the direction of blood flow;
- central region arches into the lumen of the vessel;
- Have thin lateral processes - often pinocytic vesicles within them (for transport of substances).
Lamina basalis[edit | edit source]
- Product of endothelial cells may or may not be continuous.
Subendothelial layer[edit | edit source]
- Sparse collagenous connective tissue;
- may contain smooth muscle cells;
- Elements arranged longitudinally.
Tunica media[edit | edit source]
This layer is made up of smooth muscle cells that produce intercellular matrix (glycosaminoglycans, chondroitinsulphate and proteoglycans). It also contains reticular fibres and elastic fibres. At the edges they may condense into internal and external elastic membrane (separating the tunica media from the tunica externa and tunica intima).
Tunica adventitia[edit | edit source]
The layer is composed of collagenous connective tissue, in which longitudinal collagen (mainly type I collagen) and elastic fibres predominate. Fibroblasts, adipocytes and, in larger vessels, smooth muscle cells are also found.
Vascular and nerve supply[edit | edit source]
The supply of nutrition to the wall of small blood vessels is provided by the diffusion of nutrients and oxygen from the blood flowing within that vessel. Blood vessels that are larger than 1 mm in diameter have developed a system of blood vessels within their walls. This system is called the vasa vasorum. Vasa vasorum arise as branches of the artery proper or of an adjacent artery. These vessels branch in the tunica adventitia and in the outer regions of the tunica media. Because there is a lower concentration of oxygen in the venous blood, vasa vasorum occur more frequently in the walls of veins than in the walls of arteries.
Lymphatic drainage[edit | edit source]
Lymphatic capillaries are found predominantly in the tunica adventitia of blood vessels. In veins they penetrate deeper (up to the tunica media).
Vasomotor innervation[edit | edit source]
A network of vasomotor nerve fibers (sympathetic unmyelinated) is found in the walls of most blood vessels that contain smooth muscle cells. Their chemical mediator is noradrenaline, which when released causes vasoconstriction. In arteries, most nerve fibers do not penetrate to the tunica media; noradrenaline must diffuse several micrometers to reach the smooth muscle cells of the tunica media. In veins, nerve endings are found in both the tunica adventitia and tunica media, but the total number of nerve endings is less than in arteries.
Structure of veins[edit | edit source]
The wall of the veins is less distinct and is usually thinner than the wall of the arteries. The wall thickness varies regionally, with the veins of the extremities being larger than those of the trunk. The tunica intima contains elongated polygonal endothelial cells oriented in the direction of blood flow and a thin layer of subendothelial connective tissue. The lumen is coated with a thick layer of glycocalyx. Mebrana elastica interna is not always formed and is often not continuous.
The tunica media varies regionally. It contains a very small number of muscle cells whose arrangement is highly variable. Between them are a large number of elastic and collagen fibres.
The tunica adventitia forms the thickest layer in the veins of the abdominal cavity (vena portae, vena cava inferior) and may contain longitudinally arranged smooth muscle. Compared with the arteries, the wall of the veins is less innervated but has a richer vasa vasorum, which may extend into the media.
Lymphatic vessels[edit | edit source]
Lymphatic capillaries are similar to blood capillaries with their single layer of endothelium, but are significantly more permeable due to the absence or perforation of the lamina basalis. Due to the large slits, the lymphatic capillary is thus able to accommodate even large molecules impenetrable to capillaries (e.g. chylomicrons) and thus provides additional transport function of the lymphatic system.
Lymphatic collectors are larger vessels containing characteristic, paired valves that prevent retrograde flow of lymph in physiological cases. The wall of the lymphatic collector itself already contains the tunica intima, media and adventitia, and thus resembles a blood vessel.
The lymphatic trunks are similar to small veins.
Collateral circulation[edit | edit source]
Collateral circulation is the alternate circulation around a blocked artery or vein through a different path. It may occur through a preexisting vascular connection like the Circle of Willis in the brain or through neovascularization(formation of new blood vessels). In some cases through surgical intervention collateral circulation is created artificially, for example in bypass surgery of the heart.
Hepatic cirrhosis arising from blockage in the hepatic portal vein may give rise to collateral circulation between branches of the portal and caval veins of the liver, or between the two caval veins. Consequences of newly established venous collaterals arising from portal hypertension include esophageal varices and hemorrhoids.
Used literature[edit | edit source]
- MESCHER, Anthony L. Junqueira's Basic Histology. 12. vydání. United States : McGraw-Hill Education - Europe, 2009. 480 s. ISBN 9780071630207.
- KONRÁDOVÁ, Václava, Jiří UHLÍK a Luděk VAJNER. Funkční histologie. 2. vydání. Jinočany : H & H, 2000. 291 s. ISBN 80-86022-80-3.
- PAULSEN, Douglas F. Histologie a buněčná biologie : Opakování a příprava ke zkouškám. 1. vydání. Jinočany : H & H, 2004. 433 s. ISBN 80-7319-024-9.