Testicle
It is a paired ellipsoid-shaped organ housed in the scrotum measuring 4–5 cm × 3–3.5 cm × 2.5 cm and weighing 18–25 g. The left testicle is approximately 1 cm lower than the right.
We distinguish: extremitas superior, inferior ; margo anterior, posterior ; facies medialis, lateralis .
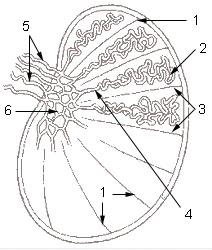
It is a compound tubular gland whose main function is the production of hormones a sperm. On the surface of the gland there is a strong fibrous sheath tunica albuginea , which covers the tunica vaginalis testis from the outside (made up of lamina visceralis tunicae vaginalis testis = epiorchium and lamina parietalis tunicae vaginalis testis = periorchium). The tunica albuginea is thickened on the dorsal side and forms the mediastinum testis , at the same time sending fibrous septa into the interior of the testis, which divide it into testis lobules.
In the testis lobule , there are seminiferous tubules (tubuli seminiferi contorti) embedded in a thin collagenous tissue, which, in addition to them, also contains blood vessels, nerves and so-called interstitial Leydig cells (production of testosterone).
From the tubuli seminiferi contorti, the sperm are drained into the tubuli recti. These merge into the rete testis, from which the efferent tubules emerge and open into the ductus epididymis.
Tubuli seminiferi contorti[edit | edit source]
The seminiferous tubules are lined with germinal epithelium, specifically multi-rowed tall cylindrical. The main function of these ducts is the formation of sperm. Beneath the epithelium is the basement membrane (BM), myoid cells, and fibroblasts – these structures are arranged beneath the BM in layers.
The germinal epithelium is made up of two types of cells:
- Sertoli cells:
- support, regulation of nutrition and protection of nourishing spermatozoa (hematotesticular barrier – barrier between the capillaries of the ducts and their interior), paracrine regulator of spermatogenesis;
- phagocytosis of residual bodies and damaged cells;
- secretion of testicular fluid;
- endocrine secretion of anti-Mullerian hormone, steroid binding hormone.
- Gametes:
- they produce sperm through a process called spermatogenesis.
- Spermatogenesis
The spaces between the channels are made up of cells: fibroblasts, mast cells, macrophages, as well as a sparse collagenous tissue in which we find nerves and blood vessels (with fenestrated capillaries). At the same time, we find Leydig cells here, in which androgens are synthesized under the influence of luteinizing hormone.
Testicular drainage[edit | edit source]
Tubuli seminiferi recti[edit | edit source]
These are the terminal parts of the contorted seminiferous tubules that join in the rete testis. Their epithelium is single-layer isoprismatic. In their course, spermatogenic cells gradually decrease.
Rete testis[edit | edit source]
A network formed by anastomosing channels in the mediastinum testis (corpus Highmori). It has the same morphology as tubuli recti and differs only in location.
Ductuli efferentes testis[edit | edit source]
It forms the head of the ductus epididymidis. It is a system of 15-20 coiled channels. They have a star-shaped lumen with an irregular shape. The epithelium is single-layered and consists of two types of cells:
- prismatic cells with kinocilia or stereocilia;
- cubic cells with microvilli.
Testicular fluid[edit | edit source]
It is formed by Sertoli cells and epithelium in the rete testis . It contains proteins, steroids, ions, and a binding protein that is specific for testosterone.
Variation[edit | edit source]
- Monorchrism
- Anorchism
- Polyorchism
They arise as a result of secondary splitting, defect or destruction of the organ.
Blood vessels and nerves[edit | edit source]
Vessels[edit | edit source]
A. testicularis , which departs from the aorta abdominalis in the L2 region (sometimes from a. renalis), enters the scrotum in the funiculus spermaticus. We can find anastomoses with the a. ductus deferentis (from the a. iliaca interna), a. cremasterica (a. epigastrica inferior).
Blood from the testicle collects in the pampiniformis plexus and continues as vv. testiculares and they open into the inferior vena cava (right) and the renal vena cava (left).
Lymph collects from the area between the ducts into the septa and into the tunica albuginea, where 4–6 collectors are formed and proceed to the nodi lumbales.
Nerves[edit | edit source]
In the testicular plexus, we find sympathetic fibers from the ganglion spermaticum from the ganglion spermaticum (at the distance of the testicular aorta from the aorta), parasympathetic fibers from the X nerve, and somatosensitive and viscerosensitive fibers leading to the Th10 segment .
Descensus testium[edit | edit source]
Testes with epididymis arise in the L1–L2 region, where they are covered by the peritoneum and attached to the wall by the mesorchium. A caudal shift in the retroperitoneum occurs already in the 3rd month prenatally, and they enter the scrotum in the 8th–10th month. lunar month.
Descent glitches[edit | edit source]
- Retentio testis, which occurs if the testicle is retained in descent. Incidence about 10%. The testes are found in the abdominal cavity, in the inguinal region, in front of the symphysis. In such a testicle, spermiogenesis and endocrine activity are impaired.
- Ectopia testis is an atypical position of a testicle that is, however, normally functional. Examples of ectopia: inguinal canal, perineum, trigonum femorale, under the skin of the penis. It occurs in 2 ‰ cases.
- Inversio testis means inversion with subsequent atypical position
Links[edit | edit source]
Related Pages[edit | edit source]
References[edit | edit source]
- KONRÁDOVÁ, Václava. Funkční histologie. H & H edition. 2000. 291 stran pp. ISBN 8086022803.
- ČIHÁK, Radomír – GRIM, Miloš. Anatomie. 2. upr. a dopl edition. Praha : Grada Publishing, 2002. 470 pp. vol. 2. ISBN 80-247-0143-X.