Median Nerve
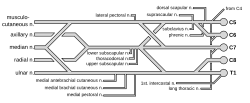
Median nerve is formed by the union of radix medialis nervi mediani (from fasciculus medialis plexus brachialis) and radix lateralis nervi mediani (from fasciculus lateralis pl. brachialis). Root innervation is C5–T1.
- Descends along the brachial artery in front of the septum intermusculare brachii mediale.
- Does not send out any branches on the arm
- In the regio cubiti, it passes between the caput humerale and ulnare musculi pronatoris teretis (canalis pronatorius in depth and continues on the forearm between m. flexor digitorum superficialis and profundus).
- In the distal third of the forearm, it is placed superficially under the fascia antebrachii between the m. palmaris longus and m. flexor carpi radialis tendons, continues under the retinaculum musculorum flexorum to the canalis carpi.
- In the canalis carpi, it is located just below the retinaculum, lateral to the m. flexor digitorum superficialis tendons.
- After leaving the canalis carpi, it enters the palm (spatium palmare medium).
Branches on forearm and hand[edit | edit source]
- Rami musculares - for m. pronator teres, m. flexor carpi radialis, m. palmaris longus and m. flexor digitorum superficialis.
- Nervus interosseus antebrachii anterior - descends along the front surface of the membrana interossea, innervates the m. flexor pollicis longus, m. flexor digitorum profundus (for the part of the muscle intended for the 2nd and 3rd fingers) and for m. pronator quadratus.
- Ramus palmaris n. mediani - a weak branch for the skin of the radial half of the carpal landscape and extends to the palm.
- Nervi digitales palmares (volares) communes I., II., III., – final branches of n. medianus in the palm, located above the flexor tendons and below the arterial arcus palmaris superficialis, project over the first to third intermetacarpal space, innervate most of the thenar muscles (+ the first 2 mm. lumbricales) and the greater part of the skin of the palm from the thumb side, at the base of the fingers, it divides in a fork-like manner into nervi digitales palmares proprii - sensitive skin branches lining the adjacent sides of the thumb, index finger, middle finger and the radial side of the ring finger, the innervation area extends to the dorsal side of the nail joints of the fingers.
- N. digitalis palmaris communis I. - gives off branches for thenar muscles (m. abductor pollicis brevis, caput superficiale m. flexor pollicis brevis, m. opponens pollicis), 3 skin branches - nn. digitales palmares proprii for both edges of the thumb and for the radial edge of the index finger.
- N. digitalis palmaris communis II. - gives off a muscular branch for m. lumbricalis I. and cutaneous nn. digitales palmares proprii for the ulnar edge of the index finger and radial edge 3 .finger.
- N. digitalis palmaris communis III. - innervates m. lumbricalis II. and gives off the skin nn. digitales palmares proprii for the ulnar edge of the 3rd finger and the radial edge of the 4th finger, the skin on the dorsal side of the nail joints 1st-3rd. finger and partly also the 4th finger.
Functions[edit | edit source]
- Motor functions: Innervates the flexor and pronator muscles in the anterior compartment of the forearm (except the flexor carpi ulnaris and ulnar half of the flexor digitorum profundus). Innervates the thenar muscles and lateral two lumbricals in the hand.
- Sensory functions: palmar cutaneous branch - innervates the lateral aspect of the palm. The digital cutaneous branch- innervates the lateral three and a half fingers on the anterior (palmar) surface of the hand.
Clinical Significance[edit | edit source]
Carpal Tunnel Syndrome (CTS)[edit | edit source]
involves compression of the median nerve within the carpal tunnel.[edit | edit source]
It is the most common mononeuropathy and is caused by an increased tissue pressure within the carpal tunnel.
Risk factors for CTS are
- diabetes
- pregnancy
- acromegaly
- hypothyroidism
- menopause
- wrist injuries
- obesity
- rheumatoid arthritis
- repetitive hand and wrist movements- This can include activities such as typing on a keyboard, using vibrating tools, or performing assembly line work.
- smoking
- medications, such as corticosteroids
- the exact underlying aetiology is not well understood.
Clinical features include numbness, tingling, and pain in the distribution of the median nerve. Importantly, the palm is usually spared – as the palmar cutaneous branch does not travel through the carpal tunnel. Symptoms are usually worse in the morning. If left untreated, chronic CTS can cause weakness and atrophy of the thenar muscles.
Tests for carpal tunnel syndrome can be performed during physical examination:
- Tinel’s sign – tapping the nerve in the carpal tunnel to elicit pain and tingling in median nerve distribution.
- Phalen’s manoeuvre – holding the wrist in flexion for 60 seconds to elicit numbness/pain in median nerve distribution.
Treatment involves
- The use of a splint
- Holding the wrist in extension overnight to relieve symptoms.
- Corticosteroid injections into the carpal tunnel can be trialled.
- Physical Therapy: Specific exercises may help strengthen muscles and improve wrist flexibility, reducing symptoms.
- Pain Management: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate pain and inflammation.
Lifestyle modifications:
- Ergonomic adjustments: Making changes to your workspace or using ergonomic tools (e.g., ergonomic keyboards, wrist rests) can help reduce strain on the wrists during activities.
- Weight management: Maintaining a healthy weight can help reduce pressure on the median nerve.
- Avoiding repetitive motions: Minimizing activities that involve repetitive or forceful wrist movements can help prevent worsening of symptoms.
Surgical decompression of the carpal tunnel may be required in severe cases. This procedure involves cutting the ligament that forms the roof of the carpal tunnel (flexor retinaculum) to relieve pressure on the median nerve. It can be performed using traditional open surgery or endoscopic techniques, which involve smaller incisions and shorter recovery times.
Damaged at the Elbow[edit | edit source]
- Cause: Supracondylar fracture of the humerus.
- The forearm constantly supinated, and wrist flexion is weak (often accompanied by adduction, because of the pull of the flexor carpi ulnaris).
- Paralysis of both the longus and brevis muscles prevents flexion at the thumb
- The lateral two lumbricals are affected, and the patient will not be able to flex at the MCP joints or extend at IP joints of the index and middle fingers.
- Lack of sensation over the areas that is innervated by the median nerve
- Atrophy of the thenar muscles. If patient tries to make a fist, only the little and ring fingers can flex completely (hand of benediction).
Damaged at the Wrist[edit | edit source]
- Cause: Lacerations just proximal to the flexor retinaculum.
- Thenar muscles and the lateral two lumbricals are paralyzed.
- Same sensory dysfunctions as above.
- The hand is held in the same position as damage at the elbow, but the forearm is unaffected.
Links[edit | edit source]
Related Articles[edit | edit source]
References[edit | edit source]
- * PETROVICKÝ, Pavel. Anatomie s topografií a klinickými aplikacemi. 1. edition. Osveta, 2002. 542 pp. ISBN 80-8063-048-8.
- The Median Nerve - Course - Motor - Sensory - TeachMeAnatomyAccessed on 26/04/2024.