Renal function replacement
There are several methods of renal replacement , some of which can be described as relatively permanent solutions and others as temporary. A group of patients can be identified who need to be provided with temporary renal replacement for an acute condition, or where the kidney damage is reversible. The second group consists of patients whose kidneys are damaged irreversibly (irreversibly) and need to replace kidney function for life.
Methods of renal replacement include:
- kidney transplantation,
- hemodialysis,
- peritoneal dialysis (lavage).
Specific indications are given for each method separately (below). In general, preparing a patient for kidney replacement should begin before renal failure occurs (from stage 4 of chronic renal failure at the latest), but often, the sooner the better. The choice of which method should be adapted to the patient - his age (IgA nephropathy often affects young people), prognosis. Kidney transplantation seems to be the most advantageous method of kidney function replacement, which can be not only the most effective (return of lost function, patient independence, prolongation of survival ...), but also the most economical.
Kidney transplantation
Kidney transplantation is indicated in any patient with chronic renal failure. At present, it is a routine method of replacing kidney function, which should be preferred over others (hemodialysis, peritoneal dialysis), both from a prognostic and economic point of view.
Indication
Transplantation should be indicated for a patient who reaches stage 4 of chronic renal insufficiency according to K/DOQI in the progression of renal failure, generally the sooner the better. It would be ideal if the patient did not have to undergo another method of replacing kidney function (hemodialysis) before the transplant.
Diseases that lead to kidney failure:
- glomerulopathy (most often IgA);
- chronic tubular diseases;
- diabetic nephropathy;
- polycystic kidney disease.
In the case of a diagnosis of type I diabetes mellitus in combination with severe (terminal) diabetic nephropathy, the kidneys are transplanted together with the pancreas as a combined pancreas transplant and kidneys, when the advantages of subsequent common immunosuppressive treatments. A kidney transplant (with subsequent immunosuppressive treatment) is also a supporting factor for the decision to perform pancreas transplantation in a diabetic.
Contraindications
- Acute or chronic infection;
- Heart Failure;
- coagulopathy;
- AIDS;
- malignant disease;
- advanced liver or lung diseases.
Donors
- Living Donors
Most often they are relatives, partners, but it is not a condition. They can also be strangers. The main factor is the voluntariness of the donation and the health of the donor. In order not to endanger the donor by removing one kidney, it is necessary to assess the function of the kidney in the future, if there is no risk of, for example, glomerulonephritis).
- Deceased (cadaveric) donors
In the Czech Republic, the so-called assumed consent for donation after death applies. If a person does not express during his life that he does not want to donate organs, he is automatically considered a donor. One of the requirements is brain death proven panangiography (2x within 30 min), then also no damage to kidney function (preserved peripheral circulation required) and cold ischemia for up to 24 hours.
Immunology
Compatibility in blood groups (AB0 system) is one of the most important. Transplantation is, however, also possible in case of mismatched blood groups (in the Czech Republic since January 2011). Antibodies in the event of a mismatch must be removed from the blood of the recipient, for example by adsorption or plasmapheresis. If there is a match in as many "HLA features" as possible and there is a low titer of lymphocytotoxic antibodies, the cross-examination will be negative. The cross-examination means that we combine the recipient's serum, the donor's lymphocytes and the complement. If the cross-test is positive, the antibodies need to be removed.
Surgical technique
- Removal of kidney;
- heterotopic placement of the graft in the right iliac fossa (vessels are connected to the iliac artery and vein, the ureter is sutured to the bladder);
- the original kidneys are usually left in place, where they gradually shrink and atrophy (the exception is polycystic kidneys, which are removed);
- in most cases, only one kidney is transplanted, rarely two (the other to the left iliac fossa), when one would not be enough to restore renal function.
Postoperative development
In 65% of cases, the kidney works immediately after transplantation. The patient is hydrated to begin urine formation.
In 25% there is a delayed development of graft function and the kidney does not work for a short time (days to weeks). After a certain time the function develops, until then hemodialysis is necessary.
In 10%, the kidney does not work at all due to thrombosis or unknown causes, for example due to primary afunction.
Statistical data
The average waiting time for a kidney is 12 months', which is much less than, for example, in the USA (3-4 years). This is due to the fact that many patients in our country are not indicated for transplantation, even if they could be. Up to 15% of kidney transplants are repeat transplants. Due to a temporary rejection of the graft, which is not a contraindication to further procedure. One-year survival of patients after transplantation exceeds 95%. Ten-year graft survival after transplantation is 50%.
Immunosuppression
- Inductive
- ATG – antithymocyte globulin – polyclonal antibodies against T lymphocytes
- basiliximab - monoclonal antibody against the IL-2 receptor on T lymphocytes (anti CD25)
- alemtuzumab (anti CD52)
- Maintenance - triple combination:
- corticosteroids (prednisone);
- basic immunosuppressants (cyclosporine A or tacrolimus);
- adjuvant immunosuppressants (azathioprine, mycophenolate mofetil).
- Anti-rejection - therapy of acute graft rejection:
- corticosteroid pulse doses of 250–500 mg of prednisone for 3–5 days, if even doses of 2–3 g of prednisone do not work, we consider corticosteroid resistant;
- in corticoresistance to polyclonal antilymphocyte antibody – ATG or monoclonal basiliximab (anti IL-2R), alemtuzumab (anti CD52).
Cyclosporin A and tacrolimus bind to cycloneurin and inhibit IL-2 expression.
Possible side effects:
Adverse effects include mainly nephrotoxicity and neurotoxicity. Tacrolimus can cause DM of the receptor type, so cyclosporine is used instead of tacrolimus in diabetics. Azathioprine is hepatotoxic and myelotoxic. It is therefore recommended to use mycophenolate mofetil instead. Last but not least, it is necessary to mention that other side effects include the threat of DM, Cushing's syndrome, osteoporosis, hyperlipidemia due to corticoids.
Complications after transplantation
- Early:
- graft rejection (hyperacute, acute) – treatment see above;
- urinary fistula;
- thrombosis of graft artery or vein;
- opportunistic infections:
- CMV pneumonitis (ganciclovir);
- pneumocystosis (cotrimoxazole);
- legionella (erythromycin).
- Late:
- hypertension (graft artery stenosis);
- chronic liver failure;
- tumors (skin, lymphomas, Grawitz);
- chronic rejection.
>Kidney transplant is indicated in every patient with chronic renal failure. It is currently a routine method of renal replacement, which should be preferred over others (hemodialysis, peritoneal dialysis), both prognostically and economically.
Indication
A patient who reaches stage 4 chronic renal failure according to K / DOQI with progression of renal failure should be indicated for transplantation, generally the sooner the better. Ideally, the patient would not have to undergo another method of renal replacement therapy (hemodialysis) prior to transplantation.
Diseases that lead to kidney failure:
- glomerulopathy (most commonly IgA);
- chronic tubular diseases;
- diabetic nephropathy;
- polycystic kidney disease.
In the case of the diagnosis of type I diabetes mellitus in combination with severe (terminal) diabetic nephropathy, the kidneys are transplanted at the same time as the pancreas as a combined pancreatic and kidney transplantation, taking advantage of subsequent joint immunosuppressive therapy. Renal transplantation (followed by immunosuppressive therapy) is also a supporting factor in the decision to have a pancreas transplant in a diabetic person.
Contraindication
- Acute or chronic infection;
- Heart Failure;
- coagulopathy;
- AIDS;
- malignancies;
- advanced liver or lung disease.
Donors
- Living donors
Most often they are relatives, partners, but it is not a condition. They can also be strangers. The main factor is the voluntariness of the donor and the health of the donor. Due to the non-threat of the donor by removing one kidney, it is necessary to prospectively assess the function of the kidney, whether there is a risk of, for example, glomerulonephritis?).
- Deceased (cadaveric) donors
In the Czech Republic, the so-called presumed consent to donation after death applies. If a person does not state during his life that he does not want to donate organs, then he is automatically considered a donor. One of the requirements is brain death proven by panangiography (2x within 30 min), then also no damage to kidney function (necessary preserved peripheral circulation) and cold ischemia for up to 24 hours.
Immunology
Compatibility in blood groups (AB0 system) is one of the most important. However, transplantation is also possible in the event of a disagreement between blood groups (in the Czech Republic since January 2011). In the event of a discrepancy, the antibodies must be removed from the recipient's blood, eg by adsorption or plasmapheresis. If there is a consensus in as many HLA traits as possible and there is a low titer of lymphocytotoxic antibodies, we will cross out the cross test. The cross-test means that we combine the recipient's serum, the donor's lymphocytes and complement. If the cross-test is positive, the antibodies need to be removed.
Surgical technique
- Kidney collection;
- placing the graft heterotopically into the right hip (vessels are attached to the iliac artery and vein, the ureter is sutured into the bladder);
- the original kidneys are usually left in a place where they gradually shrink and atrophy (with the exception of polycystic kidneys, which are removed);
- in most cases, only one kidney is transplanted, rarely two (the other in the left hip pit), if one is not enough to restore renal function.
Postoperative development
In 65% of cases, the kidney works immediately after transplantation. The patient is hydrated to begin producing urine.
In 25%, there is a delayed development of graft function and the kidney does not work for a short time (days to weeks). After a while, the function develops, until then hemodialysis is necessary.
In 10%, the kidney does not work at all due to thrombosis or unknown causes, for example due to primary dysfunction.
Statistical data
The average waiting time for the kidney is 12 months, which is much less than, for example, in the USA (3-4 years). This is due to the fact that many patients in our country are not indicated for transplantation, although they could be. Up to 15% of kidney transplants are recurrent transplants. Due to previous graft rejection, which is not a contraindication to further surgery. The one-year survival of transplant patients exceeds 95%. The 10-year graft survival after transplantation is 50%.
Immunosuppressants
- Inductive
- ATG - antithymocyte globulin - polyclonal antibodies against T lymphocytes
- basiliximab – monoclonal antibody against IL-2 receptor on T lymphocytes (anti CD25)
- alemtuzumab (anti CD52)
- Maintenance – triple combination:
- corticosteroids (prednison);
- basic immunosuppressants (cyklosporin A or tacrolimus);
- adjuvant immunosuppressants (azathioprine, mycophenolate mofetil).
- Anti-rejection – therapy of acute graft rejection:
- pulse doses of corticosteroids 250-500 mg prednisone for 3-5 days, if doses of 2-3 g prednisone do not take place, we consider corticoresistant;
- for corticoresistance polyclonal anti-lymphocyte antibody - ATG or monoclonal basiliximab (anti IL-2R), alemtuzumab (anti CD52).
Cyclosporin A and tacrolimus bind to cycloneurine and inhibit IL-2 expression.
- Possible side effects
Side effects include, in particular, nephrotoxicity and neurotoxicity. Tacrolimus can cause DM eceptor-type, so cyclosporine is used instead of tacrolimus in diabetics. Azathioprine is hepatoxic and myelooxic. It is therefore recommended to use mycophenolate mofetil instead. Last but not least, other side effects include the threat of DM, Cushing syndrome, Osteoporosis, corticosteroid hyperlipidemia.
Complications after transplantation
- Early:
- graft rejection (hyperacute, acute) - treatment see above;
- urinary fistula;
- graft artery or vein thrombosis;
- opportunistic infections:
- CMV pneumonitis (gancyklovir);
- pneumocystosis (cotrimoxazole);
- legionella (erythromycin).
- Late:
- hypertension (graft artery stenosis);
- chronic liver failure;
- tumors (skin, lymphoma, Grawitz);
- chronic rejection.
Links
Related Articles
External links
- Česká transplantační společnost pacientům - transplantace ledvin
- Koordinační středisko transplantací - transplantace ledvin
Source
- PASTOR, Jan. Langenbeck's medical web page [online]. ©2010. [cit. 24.5.2010]. <http://langenbeck.webs.com>.
References
- ČEŠKA, Richard, et al. Interna. 1. edition. Praha : Triton, 2010. 855 pp. pp. 562-564. ISBN 978-80-7387-423-0.
Hemodialysis
If the kidneys are not able to perform their basic functions (ie dialysis, resorption and Filtration) even under resting conditions, we speak of kidney failure. Dialysis is a process in which metabolic waste products (eg. potassium, urea, excess water) retained in the body during kidney failure are removed.
Principle of dialysis
Hemodialysis
The device that allows this process is known as an artificial kidney. This modern device is very technically demanding and high demands are placed on it in terms of efficiency, reliability, safety and ease of use. Hemodialysis is usually performed in a hospital or in special dialysis centers with the help of trained nurses, home dialysis is not very common in the Czech Republic, but it can be performed with the assistance of a trained family member. The patient usually undergoes hemodialysis about three times a week for four to six hours. The artificial kidney consists of three basic parts: the extracorporeal circulation of the patient's blood, the dialyzer and the circuit ensuring the flow of dialysis solution ..
Extracorporeal blood circulation
This part of the process is performed by a circuit that pumps the patient's venous blood using rotary pumps through a dialyzer under more or less the same hemodynamic conditions as in the patient's body. Because the blood here comes into contact with a surface other than the vascular endothelium, there is a risk of thrombi. Therefore, most patients are heparinized (only patients with bleeding conditions are contraindicated). The circulation also includes sensors that control the formation of air bubbles in the blood, which could be a source of embolization.
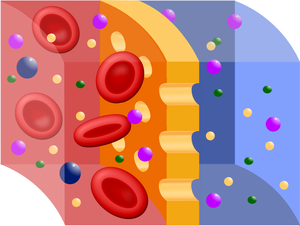
Dialyzer
The dialyzer, or capillary, is the main functional unit of the artificial kidney. The dialysis itself (physically it is a process in which substances of different sizes and solubilities are separated from each other) and the ultrafiltration of substances and water from the blood into the dialysis solution takes place through a semipermeable membrane (see picture). Membranes of animal origin (eg fish bladders, intestines) were used as filters in the first experiments, but now mainly artificial membranes, eg cellophane, glucose esters, are used or from some modern plastic (Cuprophan), which unfortunately may have the ability to stimulate the patient's immune system (of course less than the original materials) - therefore the number of dialysis may increase the risk of transplant rejection in the future. The membrane can be arranged in the dialyzer either in the form of leaves or a large number of thin tubes - the aim, of course, is to keep the effective area as large as possible. The membrane thus divides the dialyzer into a blood and a dialysate part. On one side of the membrane, the blood flows through a laminar flow, during which the erythrocytes accumulate in the flow axis and the membrane is thus more washed by the plasma. The volume flow here is approx. 200-300 ml / min. On the opposite side of the membrane, the dialysis solution flows in the opposite direction by turbulent flow, the volume flow here is about 500 ml / min. In this way, the required concentration gradient and thus rapid diffusion of oxic low-molecular substances from the patient's blood into the dialysate is achieved . Dialyzers are usually disposable, but it can be used more than once in the same patient, the efficiency does not decrease in this way (but disposable capillaries are currently used).
DDialysate circuit
This circuit involves both the preparation of the solution and its flow through the dialyzer. The dialysate is prepared by mixing a concentrated sodium bicarbonate solution prepared in a company or in a pharmacy with treated water. It is very important that the dialysis solution contains electrolytes at approximately the same concentration as in the plasma and has the correct pH, so that the acid-base balance of the patient is not disturbed . At the same time, by adding some ions, especially K+ and Ca 2+, (again using preformed solutions supplied by the company) it is possible to correct ionic imbalances. Glucose can be added to the dialysate, paradoxically in patients who are type 1 diabetics, because they are at risk of hypoglycaemia during dialysis.(due to the dialysis itself, but also the insulin dosage, which is normal for the patient, but the glucose intake is lower). It is important to control and maintain a constant temperature during the process. Consumption of dialysates in 4-6 hour hemodialysis is about 150 liters.
Types of dialysis
Acute hemodialysis
Acute dialysis is used in emergencies, where the patient's body is unable to clear itself of endogenous or exogenous toxic substances, fluid volume, or ions. Indications for acute dialysis include the following conditions:
- acute renal failure – such as rapidly progressing glomerulonephritis (RPGN),
- hyperkalaemia > 6 mmol/l, which cannot be managed with conservative therapy,
- hyperkalcemia > 3,5 mmol/l,
- hyperurikemia > 1000 μmol/l,
- uncorrectable metabolic acidosis, pH < 7,1,
- hyperhydration with heart failure,
- oligouria lasting longer than 3 days,
- intoxication with low-molecular water-soluble substances which remain in free form in the bloodstream after intoxication - eg ethylene glycol (fridex - antifreeze mixture), lithium. Other poisons can be eliminated by hemoperfusion, ie adsorption on activated carbon, which is performed by supplementing the hemodialysis device with a hemoperfusion cartridge (eg toadstool poison, paracetamol, some antidepressants).
Among the generally accepted principles of acute dialysis is to consider whether it is not possible to manage some of these conditions with conservative therapy (ion breakdowns, disorders of the internal environment), because dialysis is a method that burdens the body (cardiovascular, immune system). In acute dialysis, a central venous catheter (CKD). is used as input . Dialysis frequency as needed.
Chronic hemodialysis
Chronic hemodialysis is used in patients who have usually developed renal failure despite chronic renal insufficiency (stage 5 according to K / DOQI), a condition in which even under basal conditions their body is unable to get rid of excess metabolites, fluid volume and correct internal environment (pH, ions). Patients usually go on dialysis 3 times a week, dialysis for 4-6 hours. For vascular access is preferred arteriovenous shunt between a. radialis and v. cephalica: If is contraindicated (heart failure), at a central venous catheter into v. jugularis. This treatment is for life or kidney transplantation.
Indications for dialysis (in diabetics previously)[1]:
- urea > 30 mmol/l,
- creatinine 600–800 μmol/l,
- creatinine clearance < 0,25 ml/s.
Diseases that lead to hemodialysis are:
- diabetic nephropathy,
- hypertensive nephropathy,
- chronic glomerulonephritis,
- rapidly progressing glomerulonephritis (RPGN) – when it reaches irreversible fibrotic changes,
- autosomal dominant polycystic kidney disease.
In patients for whom dialysis is expected, we should first contact the Transplant Coordination Center or the IKEM Transplant Surgery Clinic to ensure the possibility of kidney transplantation as soon as possible. We should also treat anemia (erythropoietin), which most patients with renal failure suffer from, and carry out preventive vaccination against hepatitis B (the development of which is a reason for delaying transplants and shortening survival). Acute complications of hemodialysis include hypotension (from a sudden loss of circulating fluid volume), convulsions (decrease in Na+, K+, Ca2+), arrhythmias (sudden hypokalaemia) and bleeding at the vascular access site (related to heparinisation). Chronic complications of hemodialysis include cardiovascular complication (CHD, myocardial infarction, CMP, hypertension, kwhich are more common in dialysis patients than in the general population), infections (hepatitis B and hepatitis C), amyloidosis (beta2-mikroglobulin).
Complications in chronic dialysis
- heart failure
- infection
- anemia
Links
Reference
- ↑ ČEŠKA, Richard, et al. Interna. 1. edition. Praha : Triton, 2010. 855 pp. pp. 558. ISBN 978-80-7387-423-0.
References
- BENEŠ, Jiří – STRÁNSKÝ, Pravoslav – VÍTEK, František. Základy lékařské biofyziky. 2. edition. Praha : Karolinum, 2007. 201 pp. ISBN 978-80-246-1386-4.
- HRAZDIRA, Ivo – MORNSTEJN, Vojtěch. Lékařská biofyzika a přístrojová technika. 1. edition. Brno : Neptun, 2001. ISBN 80-902896-1-4.
- ČEŠKA, Richard, et al. Interna. 1. edition. Praha : Triton, 2010. 855 pp. pp. 558-560. ISBN 978-80-7387-423-0.
Peritoneal dialysis
Peritoneal dialysis (PD) is a dialysis method of kidney function replacement. PD uses the peritoneum as a membrane through which fluids and solutes (electrolytes, urea, glucosa, albumin, osmotically active particles, and other small molecules) are exchanged from the blood. Dialysis fluid is delivered to the abdominal cavity through a permanently inserted catheter.
Dialysis takes place either every night during sleep (automatic peritoneal dialysis) or during regular changes during the day (continuous outpatient peritoneal dialysis). PD is used as an alternative to hemodialysis, although significantly less often in many countries (eg the USA). It is comparatively safe, but significantly less expensive in most countries of the world. The main advantage of PD is the ability to undergo treatment without visiting a medical facility. The most common complication of PD is infection through a permanently inserted catheter in the abdominal cavity.
Design and types of peritoneal dialysis
The fluid enters the abdominal cavity through a peritoneal catheter, which is inserted permanently through the abdominal wall below the level of the navel. The patient can infuse and discharge the dialysis solution into the abdomen on its own and several times a day, up to 4 times during continuous ambulatory peritoneal dialysis (CAPD), where the fluid in the peritoneal cavity is usually left for 6 hours. The used and contaminated dialysis solution is drained out and replaced with new and clean dialysate (if the patient dialys several times a day).
Automated peritoneal dialysis (APD) using the device reduces the number of exchanges to one day and replaces frequent changes at night, [1], the patient connects to the exchange device automatically before going to bed and his sleep is not affected.
- Principle of peritoneal dialysis
Best practises
According to best practice, before starting peritoneal dialysis treatment, it is necessary to evaluate how well the patient understands the PD process itself, instruct him on proper catheter care and complete any missing information. The patient should be constantly monitored to ensure that dialysis is performed properly and should be examined regularly for any complications. The patient should also be properly instructed in the importance of infection prevention and should develop an appropriate treatment plan.[2]
- In preparation for the procedure, the abdominal cavity is cleaned and a catheter is surgically inserted with one end in the abdominal cavity and the other protruding from the skin. [3]
- Before each infusion, the catheter must be cleaned and the flow verified in both directions.
- In about ten to fifteen minutes, 2-3 liters of dialysis fluid (so-called dialysate) are introduced into the abdominal cavity . Its total volume can reach up to 3 liters and drugs can be added to the fluid just before administration.
- The fluid is left in the abdominal cavity for a certain period of time (so-called delay ), when waste products pass into it from the vascular system through the peritoneum. After this delay (usually 4-6 hours depending on the treatment, [4][5]the fluid is drained and replaced with fresh. This can take place automatically during sleep (automated peritoneal dialysis, APD) or during the day, leaving two liters of dialysate in the abdomen at all times and changing four to six times a day (continuous outpatient peritoneal dialysis, CAPD).
The fluid usually contains sodium, chloride, lactate or bicarbonate and a high percentage of glucose to ensure hyperosmolarity.
The intensity of dialysis depends on the amount of dialysate, the regularity of its exchange and the concentration of the solution. For APDs, there are 3-10 exchanges per night, while for CAPDs there are four exchanges per day, with a dialysate volume of between 2-3 liters and a residence time of 4-8 hours.
The visceral part occupies about four-fifths of the total peritoneal area, but the parietal peritoneum is more important for PD. The principle of membrane dialysis is explained by two complementary models - a three-pore model (where molecules - proteins, electrolytes or water - permeate the membrane and "sieves" them depending on pore size) and a distributed model (which emphasizes the role of capillaries and ability to increase number of active capillaries participating in the PD).
High glucose concentration stimulates osmotic filtration of fluid from the peritoneal capillaries into the abdominal cavity. Glucose passes from the dialysate into the blood (capillaries) relatively quickly. After a 4–6 hour delay, the osmotic glucose gradient usually drops too low for osmotic filtration to continue. The dialysate is therefore absorbed back from the abdominal cavity into the capillaries due to the colloidal osmotic pressure of the plasma , which exceeds the colloidal osmotic pressure in the peritoneum by approximately 18–20 mmHg (cf. Starling's mechanism).[6] Lymphatic absorption also contributes to some extent to the reabsorption of fluid from the abdominal cavity into plasma. In patients with high water permeability (UF coefficient) of the peritoneal membrane, there may be increased reabsorption of fluid from the peritoneum at the end of the delay.
The ability of small particles and fluids to exchange between Peritoneum and Plasma can be classified as high (fast), low (slow), or medium. There is good diffusion in patients withfast exchange (easy exchange of small molecules between blood and dialysate, some improvement in results can be achieved by more frequent, shorter delays than in APD), while patients with slow exchange show a higher UF filtration rate (due to slower glucose reuptake from abdominal cavities, where better delays with higher fluid volume show better results), although in practice both types of patients can generally be treated with appropriately adjusted APD or CAPD.[7]
Although there are several different shapes and sizes of catheters that can be used, different catheter insertion sites, number of cuffs, and attachment, there are no known differences in morbidity, mortality orinfections, but the information is not good enough to draw definitive conclusions.[8]
Complication
The volume of dialysate pumped and the patient's weight are monitored. If more than 500 ml of fluid remains or if 1 liter of fluid is lost during three consecutive treatments, the patient's attending physician is notified. Excessive fluid loss can lead to hypovolemic shock or hypotension. Excessive fluid retention can lead to hypertension and swelling.
The colour of the fluid discharged is also monitored : under normal circumstances it is pinkish for the first four cycles and then clear or pale yellow. The presence of a pink or bloody discoloration indicates bleeding into the abdominal cavity, faeces indicate bowel perforation, and cataracts can indicate infection.
The patient may also experience pain or discomfort,if the dialysate is too acidic, too cold, or soaked. Diffuse pain and turbid fluid discharge may indicate infection. Severe pain in the rectum or perineum may be the result of an improperly inserted catheter. The dialysate can also increase the pressure on the diaphragm, making breathing difficult, and constipation can restrict fluid flow through the catheter.
A potentially fatal complication that is estimated to occur in approximately 2,5 % of patients, is encapsulating peritoneal sclerosis, in which the bowel becomes obstructed due to a thick layer of fibrin in the peritoneum.[9]
The primary osmotic agent in a dialysate is usually glucose, which can lead to peritonitis, renal and peritoneal membrane failure, and other health complications. Acidity, high concentrations and the presence of lactate and especially glucose breakdown products in solution can contribute to such problems. Solutions that are neutral, use bicarbonate instead of lactate, and contain fewer glucose breakdown products are safer, but there are no studies to confirm this. [10]
Risks and benefits
PD is less effective in removing fumes from the body than hemodialysis, and the presence of a catheter poses a risk of peritonitis by possibly introducing bacteria into the abdomen.[4] There is insufficient evidence of the best treatment for PD-related peritonitis, although direct infusions of antibiotics into the abdomen show slightly better results than intravenous administration. There is no clear benefit from other frequently used treatments, such as regular peritoneal lavages or urokinase use.[11]
Catheter insertion site infection may also occur. Prophylaxis with nasal mupirocin, which does not affect peritonitis , may reduce the number of such infections.[12] Infections occur on average once every 15 months (0.8 episodes per patient per year), but significantly less frequent in many settings - once every 40 months or more compared to hemodialysis, PD allows the patient better mobility, due to its Due to their ongoing nature, there are fewer fluctuations in symptoms and phosphates are better removed , but large amounts of Albumin, are also removed from the body , which requires constant monitoring of nutritional status.
In most countries of the world, the cost of PD is generally lower than that of HD, with the price difference being most pronounced in developed countries.[13]
So far, not enough research has been done to compare the risks and benefits of CAPD and APD. Cochrane, an independent professional organization, compared the results of three smaller clinical trials and found no difference in clinically significant parameters (ie morbidity and mortality) in patients with end-stage renal disease, nor the benefit of either method in maintaining kidney function. The results suggest that APD may have psychosocial benefits in younger patients and those who are employed or studying.[14]
Other complications include hypotension (due to increased fluid exchange and sodium loss), pain in the hips and hernias, or fluid leakage due to increased intra-abdominal pressure. PD can also be used in patients with kardiovascular instability because it does not cause rapid and significant changes in body fluids, and in patients with type 1 Diabetes due to the inability to control blood sugar levels through a catheter. Possible risks are also hypertriglyceridemia and obesity due to the large amount of glucose in the dialysis fluid, which can supply the body with 2000–5000 kJ per day.[15]
Of the three types of connections and fluid exchange systems (standard, with two bags and with a Y-coupling, the latter two working with two bags and only one catheter connection, with the Y-coupling kit being the only Y-shaped connection between the discharge bags, flushing and impregnation) systems with two bags and a Y-joint show better results in preventing peritonitis than conventional systems.[16]
Extension of the method
According to a 2004 global survey, approximately 11 % of end-stage renal disease patients were treated withPD compared to significantly more common hemodialysis. In Hong Kong and Mexico, PD is more common than the global average - in Mexico it is applied to most patients (75 %) – while in Japan and Germany, PD use is below the world average.[17]
Improvised dialysis
Peritoneal dialysis can be performed improvised, eg in combat conditions or in catastrophes, using surgical catheters and dialysate made from commonly available infusion solutions to provide temporary replacement of renal function in patients for whom there is no other option.
Indication
This method is advantageous for young patients, who do not have to go to the hospital regularly for hemodialysis, so they can continue their normal activities (work, study). We also use peritoneal dialysis in children and circulatory unstable patients, where we cannot provide stable and suitable conditions for hemodialysis.
Contraindication
Peritoneal dialysis is not indicated in patients with extensive peritoneal adhesions, hernias, colostomies, active bowel disease (Crohn's disease), ascites or in non-cooperating patients.
Complication
The most common complication is infection – usually staphylococcal peritonitis clogged with a catheter (general and local ATB therapy). Over time, peritoneal dialysis can thicken the peritoneum. This disrupts his diffusion function and the patient should be transferred to hemodialysis.
Links
Source
- ↑ ČEŠKA, Richard, et al. Interna. 2. edition. Praha : Triton, 2015. 909 pp. ISBN 978-80-7387-895-5.
- ↑ Wood, M; et al. (2008-08-01). "Nephrology Nursing Standards and Practice Recommendations" (PDF). Canadian Association of Nephrology Nurses and Technologists. Retrieved 2010-09-08.
- ↑ Haralampos V. Harissis et al. A new simplified one port laparoscopic technique of peritoneal dialysis catheter placement with intra-abdominal fixation. The American Journal of Surgery 192 (2006) 125–129 https://www.youtube.com/watch?v=0MuJURb7vpg
- ↑ a b Crowley, LV (2009). An Introduction to Human Disease: Pathology and Pathophysiology Correlations. Jones & Bartlett Publishers. pp. 507–509. ISBN 0-7637-6591-0.
- ↑ McPhee, SJ; Tierney LM; Papadakis MA (2007). Current medical diagnosis and treatment. McGraw-Hill. pp. 934–935. ISBN 0-07-147247-9.
- ↑ Rippe, B, Venturoli, D, Simonsen, O, de Arteaga, J (2004). "Fluid and electrolyte transport across the peritoneal membrane during CAPD according to the three-pore model.". Perit Dial Int 24: 10–27. PMID 15104333.
- ↑ Daugirdas, JT; Blake PG; Ing TS (2006). "Physiology of Peritoneal Dialysis". Handbook of dialysis. Lippincott Williams & Wilkins. p. 323.
- ↑ Strippoli, GFM; Tong A; Johnson DW; Schena FP; Craig JC (2004). Strippoli, Giovanni FM, ed. "Catheter type, placement and insertion techniques for preventing peritonitis in peritoneal dialysis patients". Cochrane Database of Systematic Reviews 4: CD004680.doi:10.1002/14651858.CD004680.pub2. PMID 15495125.
- ↑ Kawanishi, H.; Moriishi, M. (2007). "Encapsulating peritoneal sclerosis: prevention and treatment". Peritoneal dialysis international : journal of the International Society for Peritoneal Dialysis. 27 Suppl 2: S289–S292. PMID 17556321.
- ↑ Perl, J.; Nessim, S. J.; Bargman, J. M. (2011). "The biocompatibility of neutral pH, low-GDP peritoneal dialysis solutions: Benefit at bench, bedside, or both?". Kidney International 79 (8): 814–824. doi:10.1038/ki.2010.515. PMID 21248712.
- ↑ Ballinger, AE; Palmer, SC; Wiggins, KJ; Craig, JC; Johnson, DW; Cross, NB; Strippoli, GFM (26 April 2014). "What is the best treatment to manage peritonitis in people on peritoneal dialysis?". Cochrane Database of Systematic Reviews 4: CD005284.doi:10.1002/14651858.CD005284.pub3. PMID 18254075.
- ↑ Strippoli, GFM; Tong A; Johnson DW; Schena FP; Craig JC (2004). Strippoli, Giovanni FM, ed. "Antimicrobial agents for preventing peritonitis in peritoneal dialysis patients". Cochrane Database of Systematic Reviews 4 (4): CD004679. doi:10.1002/14651858.CD004679.pub2.PMID 15495124.
- ↑ Karopadi, AN; Mason G; Rettore E; Ronco C (2013). Zoccali, Carmine, ed. "Cost of peritoneal dialysis and haemodialysis across the world". Nephrol Dial Transplant 28: 2553–69. doi:10.1093/ndt/gft214. PMID 23737482.
- ↑ Rabindranath, KS; et al. (2007). Rabindranath, Kannaiyan S, ed. "Continuous ambulatory peritoneal dialysis versus automated peritoneal dialysis for end-stage renal disease". Cochrane Database of Systematic Reviews 2 (2): CD006515. doi:10.1002/14651858.CD006515.PMID 17443624.
- ↑ Ehrman, JK; Gordon P; Visich PS; Keteyian SJ (2008). Clinical Exercise Physiology. Human Kinetics. pp. 268–269. ISBN 0-7360-6565-2.
- ↑ Daly, C; Khan, I; Rabindranath, KS; Vale, L; Wallace, SA (13 August 2014). "Y-set and double bag systems offer the most protection against peritonitis during continuous ambulatory peritoneal dialysis (CAPD)". Cochrane Database of Systematic Reviews (8): CD003078.doi:10.1002/14651858.CD003078.pub2. PMID 11406068.
- ↑ Grassmann, A; Gioberge S; Moeller S; Brown G (2005). "ESRD patients in 2004: global overview of patient numbers, treatment modalities and associated trends". Nephrology Dialysis Transplantation 20 (12): 2587–2593. doi:10.1093/ndt/gfi159. PMID 16204281.
Reference
- KLENER, Pavel, et al. Vnitřní lékařství. 3. edition. Praha : Galén, 2006. 1158 pp. ISBN 80-7262-430-X.
- KYMPLOVÁ, Jaroslava. Katalog metod v biofyzice [online]. [cit. 2012-09-20]. <https://portal.lf1.cuni.cz/clanek-793-katalog-metod-v-biofyzice>.
- ČEŠKA, Richard, et al. Interna. 1. edition. Praha : Triton, 2010. 855 pp. pp. 558−560. ISBN 978-80-7387-423-0.
Links
External links
- Česká transplantační společnost pacientům - transplantace ledvin
- Koordinační středisko transplantací - transplantace ledvin
Source
- PASTOR, Jan. Langenbeck's medical web page [online]. ©2010. [cit. 24.5.2010]. <http://langenbeck.webs.com>.
Reference
- ČEŠKA, Richard, et al. Interna. 1. edition. Praha : Triton, 2010. 855 pp. ISBN 978-80-7387-423-0.
- BENEŠ, Jiří – STRÁNSKÝ, Pravoslav – VÍTEK, František. Základy lékařské biofyziky. 2. edition. Praha : Karolinum, 2007. 201 pp. ISBN 978-80-246-1386-4.
- HRAZDIRA, Ivo – MORNSTEJN, Vojtěch. Lékařská biofyzika a přístrojová technika. 1. edition. Brno : Neptun, 2001. ISBN 80-902896-1-4.