Atrial fibrillation
Atrial fibrillation (atrial fibrillation, FS, FiS) is the most common arrhythmia worldwide. It is a tachyarrhythmia with disordered atrial activity with absolute irregularity of impulse transmission to the ventricles, which is associated with increased morbidity and mortality.
Atrial fibrillation (atrial fibrillation, FS, FiS) is the most common arrhythmia worldwide. It is a tachyarrhythmia with disordered atrial activity with absolute irregularity of impulse transmission to the ventricles, which is associated with increased morbidity and mortality.
Atrial fibrillation:
Atrial fibrillation 2:
FS Types[edit | edit source]
We distinguish 4 basic types of FS:[1]
- first documented attack;
- paroxysmal - FS occurs in attacks that end spontaneously, usually within 48 hours,; or episodes lasting up to 7 days terminated by cardioversion;
- persistent – AF does not end spontaneously, it is necessary to perform pharmacological or electrical cardioversion;
- permanent - neither cardioversion nor antiarrhythmic treatment leads to the establishment of sinus rhythm.
Sinus Rhythm:
Etiopathogenesis[edit | edit source]
The occurrence and maintenance of atrial fibrillation are usually caused by rapid bursts of atrial extrasystoles, most often coming from the pulmonary veins, and structural changes in the atrial musculature, which occurs due to aging. heart diseases (IHD, heart failure, valvular defects).
With mitral valve defects, there is an overload of the left atrium. Similarly, with arterial hypertension, there is hypertrophy of the left ventricle and, subsequently, a failure of its filling and a rise in pressure in the left atrium.
Mezi predisponující faktory řadíme:
- arterial hypertension,
- ischemic heart disease,
- valvular defects,
- heart insufficiency,
- conditions after cardiosurgical procedures,
- acute pericarditis,
- thyrotoxicosis,
- mineral imbalance.
Atrial fibrillation also occurs more often in patients with COPD, obstructive sleep apnea, chronic kidney disease, diabetes mellitus, obesity , increased alcohol consumption, but also during regular intensive exercise.
Symptoms[edit | edit source]
The atrium does not contract, so it is not used in the last phase of diastole, when blood is actively pushed into the ventricle. Symptoms of atrial fibrillation are based on a decrease in cardiac output:
- stuffiness;
- angina;
- palpitation;
- presyncope.
Atrial fibrillation can be asymptomatic and then the first manifestation is a systemic embolization.
Diagnostics[edit | edit source]
Pulse is irregular. Diagnostics mainly hinge on EKG. We can observe these abnormalities:
- missing P wave – they are replaced by irregular isoelectric line or fibrillation waves;
- QRS complexes are narrow;
- R–R interval is irregular → irregular atrial action;
- heart rate is between 80–180/min.
Atrial fibrillation is characterized by ``asynchronous contraction of atrial muscle fibers (``lack of P waves). A large number of impulses are generated in the atrial myocardium, which travel to the AV node. The rate of the atria tends to be ``300-600/min, while the rate of the ventricles is 80-180/min. The AV node blocks the transfer of most atrial contractions to the ventricles. It thus protects the chambers from their exhaustion. The AV node works on the "all or nothing" principle → only impulses with the appropriate intensity pass through. Such excitations occur irregularly in the atria, so that the ventricles also contract irregularly (R–R interval is irregular; heart rate varies between 80–180/min). The transition from the atria to the ventricles takes place physiologically via the AV node and the bundle of Hiss (QRS complexes are slender).
At the first occurrence of atrial fibrillation, it is necessary to rule out possible causes of tachycardia, e.g. AMI, PE, thyrotoxicosis, hypokalemia, [[ Anemia], infection.
Differential diagnosis[edit | edit source]
In terms of differential diagnosis, it is necessary to differentiate:
- typical atrial flutter (type 1);
- atypical atrial flutter (type 2).
Complications[edit | edit source]
- Creation of a mural thrombus' and subsequent embolization (primarily to the CNS). Thrombi most often form in the ears.
- Tachycardia cardiomyopathy, left ventricular dysfunction, heart failure
- Cognitive impairment and vascular dementia. They can also develop in anticoagulated patients with AF. Lesions in the white matter of the brain are seen more often in patients with AF than in patients without AF.
Treatment[edit | edit source]
In the treatment of atrial fibrillation, we try to:
- establishing and maintaining an optimal heart rate' (ventricular rate);
- establishment and maintenance of sinus rhythm';
- elimination of thromboembolic complications'.
Establishing and maintaining an optimal heart rate[edit | edit source]
Atrial fibrillation is classified among the so-called tachyarrhythmias. The heart rate reaches values of up to 180/min.
Medicines with a negative chronotropic effect are used to slow down the heart rate.[2]
- β-blockers – negative inotropic, chronotropic and dromotropic effect. They are not suitable for patients with heart failure, AV block or sick sinus syndrome. Their advantage is the rapid onset of effect. The most frequently used preparations are metoprolol, atenolol and bisoprolol.
- Calcium channel blockers - negative inotropic, chronotropic and dromotropic effect, not suitable for patients with heart insufficiency, AV-block or sick sinus syndrome . Their advantage is the rapid onset of effect. The most frequently used drugs are diltiazem and verapamil.
- Digoxin – positive inotropic effect, negative dromotropic and negative chronotropic effect, is suitable for elderly patients with heart insufficiency and little physical activity. Its disadvantage is the slow onset of effect.
Establishing and maintaining sinus rhythm[edit | edit source]
- Establishment of sinus rhythm
We use pharmacological or electrical cardioversion to establish sinus rhythm:
- Chemical (pharmacological) cardioversion: propafenone, amiodarone (to perform chemical cardioversion, it is necessary to hospitalize the patient and continuously monitor the ECG).[2]
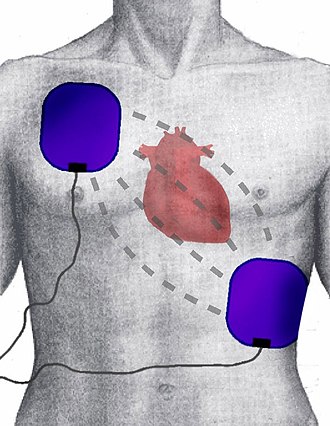
- Electrical cardioversion (external or internal): external electrical cardioversion can be performed on an outpatient basis (without the need for hospitalization). Using a biphasic 'synchronized (with QRS so that the discharge does not enter the vulnerable phase and does not cause ventricular fibrillation) discharge, we choose an energy of 70-170 J. Electrical cardioversion is more effective and safer compared to chemical cardioversion.[3]
Cardioversion can only be performed with the prevention of systemic embolization. The only exception is hemodynamically intolerable arrhythmias. Alternatively, thrombus in the left atrial appendage can be ruled out by TEE and anticoagulation is started only after cardioversion.
- Maintenance of sinus rhythm
We mainly use antiarrhythmics class Ic (propafenone, flecainide) and class III (amiodarone, sotalol).
Catheter ablation [4][edit | edit source]
In the case of pharmacological treatment, a so-called neselective radiofrequency ablation of the AV node followed by a pacemaker implantation or selective radiofreqeuncy ablation.
In the case of non-selective radiofrequency ablation, we introduce the ablation catheter into the right heart via the femoral vein. A radiofrequency current is applied to the area of the AV junction, thereby artificially inducing bradycardia as a result of complete AV blockade with preserved stable junctional rhythm. We then implant a heart pacemaker. This procedure is performed only in highly symptomatic patients resistant to pharmacological treatment.
The essence of selective radiofrequency ablation is the isolation of pulmonary veins after the introduction of a catheter into the right atrium and subsequent transseptal puncture. Due to the higher risk of complications, this method is mainly used in patients with symptomatic drug-resistant paroxysmal atrial fibrillation.[5]
Elimination of thromboembolic complications[edit | edit source]
The risk of thromboembolic complications is evaluated according to the CHA2DS2-VASc score. In patients with a high risk of thromboembolism (men with a score ≥ 2, women ≥ 3), anticoagulation therapy is indicated.[6] For patients with medium risk (men ≥ 1, women ≥ 2), we use treatment according to the patient's preferences. NOACs are used as first-line drugs, followed by warfarin.
The HAS-BLED score is used to determine the risk of bleeding complications during anticoagulant treatment in patients with AF. In patients with an increased risk of bleeding, a reduced dose of anticoagulants is used.
Antiplatelet therapy is not recommended unless there is another indication, e.g. CAD, etc.
An alternative to the prevention of thromboembolic complications is the use of obliteration of the left atrial appendage with an occluder or surgical ligation of the atrial appendage.
Links[edit | edit source]
Related Articles[edit | edit source]
- CHA2DS2-Sc and HAS-BLED Calculator
- Heart rhythm disorders • Practice EKG
- Atrial Flutter • Ventricular Fibrillation
- Cardiac conduction system
- Antiarrhythmics • Effect of drugs on heart rhythm
External links[edit | edit source]
- Atrial fibrillation - Free ECG book
- Atrial Fibrillation Animation
- Irregular irregular rhythms (atrial fibrillation, multifocal atrial tachycardia, etc.)
Reference[edit | edit source]
- ↑ ŠIHÁK, R – HEINC, P. Recommendations for the treatment of patients with atrial fibrillation. Cor et Vasa [online]. 2004, y. 46, vol. 5, p. K 67–K77, Available from <https://www.kardio-cz.cz/data/upload/Doporuceni_pro_lecbu_pacient_s_fibrilaci_sini_2004.pdf>. ISSN 1803-7712.
- ↑ Jump up to: a b LUKL, Jan. Treatment of atrial fibrillation and flutter. Internal medicine for practice [online]. 2001, y. 4, no. 1, p. 8-12, Available from <http://www.solen.cz/pdfs/int/2001/01/03.pdf>. ISSN 1803-5256.
- ↑ BYTESNÍK, Jan – LUKL, Jan. Recommended procedures for the diagnosis and treatment of cardiac arrhythmias - 3. Cor et Vasa [online]. 1998, y. 40, vol. 6, p. K216-K222, Available from <https://www.kardio-cz.cz/data/upload/Doporucene_postupy_pro_diagnostiku_a_lecbu_srdecnich_arytmii_1998.pdf>. ISSN 1803-7712.
- ↑ TÁBORSKÝ, Miloš. Neselektivní ablace AV-uzlu: nové aspekty v době kurativní léčby fibrilace síní a srdeční resynchronizační terapie. Kardiologická revue [online]. 2006, y. 12, p. 10-12, Available from <https://www.kardiologickarevue.cz/casopisy/kardiologicka-revue/2006-supplementum/neselektivni-ablace-av-uzlu-nove-aspekty-v-dobe-kurativni-lecby-fibrilace-sini-a-srdecni-resynchronizacni-terapie-33131>. ISSN 1801-8653.
- ↑ CZECH, Richard, et al. Intern. 1. edition. Prague : Triton, 2010. 855 pp. pp. 480-481. ISBN 978-80-7387-423-0.
- ↑ ŠIHÁK, R – HEINC, P. Recommendations for the treatment of patients with atrial fibrillation. Cor et Vasa [online]. 2004, y. 46, vol. 5, p. K 67–K77, Available from <https://www.kardio-cz.cz/data/upload/Doporuceni_pro_lecbu_pacient_s_fibrilaci_sini_2004.pdf>. ISSN 1803-7712.
References[edit | edit source]
- VACHEK, Jan – MÓTAŇ, Vit – ZAKIYANOV, Oscar, et al. Acute conditions in internal medicine. 1. edition. Maxdorf, 2018. ISBN 9788073455507.
- HAMPTON, John R. ECG briefly, clearly, clearly. 6. edition. Grada, 2005. 149 pp. ISBN 80-247-0960-0.
- NOT USED, Peter. , et al. The role of cardioversion in the treatment of atrial fibrillation. Cardiology review [online]. 2002, vol. 2, p. 109-113, Available from <http://www.kardiologickarevue.cz/pdf/kr_02_02_09.pdf>. ISSN 1801-8653.
- HAMAN, Peter. EKG Learning Site : ECG Basics [online]. [cit. 2010-11-01]. <http://www.ekg.kvalitne.cz/tvorba.htm#Fibrillace%20s%C3%ADn%C3%AD>.
- HELLO, Robert. Cardiology ring. III. internal clinic of VFN and 1st Faculty of Medicine of the University of Prague in Prague, 2009.
- VILICUS, Zdeněk. Interpretation of ECG at rest and during exercise. Institute of Physical Education Medicine 1. LF UK and VFN; 2010.
- CZECH, Richard, et al. Intern. 2. edition. Prague : Triton, 2015. 897 pp. pp. 98-102. ISBN 978-80-7387-895-5.