Disorders of Calcium And Phosphate Metabolism
Disorders of calcium phosphate metabolism are accompanied by abnormal levels of calcium and/or phosphorus and include disorders in the absorption, transport, storage and utilization of these minerals.
Calcium phosphate metabolism[edit | edit source]
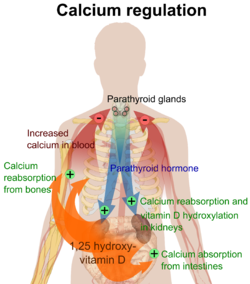
99% of calcium is stored in mineralized bone mass and 1% is part of the body's internal environment in the form of calcium ions. Calcemia is mainly regulated by vitamin D and parathyroid hormone , and to a lesser extent by calcitonin .
The exogenous source of vitamin D is mainly fish, and the endogenous source is 7-dehydrocholesterol , which is transformed in the skin by the effect of UV radiation into cholecalciferol (vitamin D 3 ) → in the liver to calcidiol (25(OH)D 3 ) → in the kidneys to calcitriol (1 ,25(OH) 2 D 3 ), the most effective metabolite.
Parathyroid hormone (PTH) is a peptide hormone produced by the parathyroid glands. Synthesis and secretion is controlled by a simple feedback loop – during hypocalcemia, the release of PTH into the blood increases.
Calcitonin (thyrocalcitonin) is a peptide hormone produced by the parafollicular (C-cells) of the thyroid gland; the concentration of calcitonin increases with hypercalcemia, so it has a hypocalcemic effect.[1][2]
| Vitamin D | Parathyroid hormone | calcitonin | |
|---|---|---|---|
| Kidney | ↑ reabsorption of Ca 2+ and phosphates | ↑ resorption of Ca 2+ and excretion of phosphates,
stimulates the production of calcitriol |
↑ excretion of Ca 2+ ,
↑ excretion of phosphates |
| Bone | bone mineralization
high levels, on the other hand, decalcify |
bone resorption (osteoclast activation),
calcemia and phosphatemia rise |
inhibition of osteoclasts,
deposition of Ca 2+ in bones |
| Intestine | stimulates resorption of Ca 2+ and phosphates | stimulates the production of calcitriol
→ stimulates the resorption of Ca 2+ and phosphates |
- |
🔬 See Calcium-Phosphate Metabolism for more detailed Information
Disorders of calcium phosphate metabolism in children[edit | edit source]
Hypocalcemia[edit | edit source]
- serum calcium < 2.0 mmol/l.[1]
- Clinical manifestations:
- acute: apnea in newborns, tetany, convulsions (resemble epilepsy), muscle spasms, laryngospasm, dysarthria from spasm of the masseters, carpopedal spasms, prolonged QT interval on ECG
- latent tetany: Chvostk's sign (a tap on the face in front of the jaw joint at the site of the nervus facialis leads to a twitch in the face), Trousseau's sign (an inflated tonometer cuff on the arm causes the obstetric hand sign within a few minutes)
- chronic: hair and nail growth disorders, possibly deposition of calcium in soft tissues → cataract, basal ganglia calcification, nephrocalcinosis, subcutaneous calcification in places of hematomas and minor trauma.
- Differential diagnosis
- reduced secretion or reduced effects of PTH: hypoparathyroidism ( DiGeorge syndrome , activating mutation of the calcium sensing receptor, autoimmune destruction – autoimmune polyglandular syndrome type I , iatrogenic damage during thyroid surgery), pseudohypoparathyroidism (target organ resistance to PTH), hypomagnesemia
- vitamin D deficiency or dysfunction: vitamin D deficiency rickets , vitamin D-dependent rickets type I and II;
- hyperphosphatemia : chronic renal insufficiency , cytostatic treatment, excessive supply of phosphates;
- malabsorption syndrome.[1]
Hypercalcemia[edit | edit source]
- serum calcium > 2.6 mmol/l.
- Clinical manifestations
- reduced motility of the gastrointestinal tract, constipation, loss of appetite, nausea, vomiting,
- neurological symptoms: muscle weakness, somnolence, confusion, hallucinations, coma,
- cardiovascular symptoms: hypertension, tachycardia, ECG changes.
- Differential diagnosis
- hyperparathyroidism : adenoma of the parathyroid gland (the most common cause of hypercalcemia), inactivating mutation of the calcium sensing receptor;
- increased resorption of calcium by the intestine and/or kidneys : phosphate deficiency (premature children), treatment with thiazide diuretics, vitamin D, A intoxication, sarcoidosis ;
- increased resorption of calcium from bone : thyrotoxicosis , immobilization, malignancies, bone metastases, paraneoplastic secretion of PTH or PTH-related protein.[1]
Rickets[edit | edit source]
- bone mineralization disorder due to lack of vitamin D or calcium or disorders of their metabolism:
- vitamin D deficiency rickets (children) / osteomalacia (adults)
- it arises when there is a lack of vitamin D and/or calcium;
- risk groups: fully breastfed dark-skinned children whose parents do not provide vitamin D, dark skin, strict vegetarian (vegan) diet, malabsorption syndromes with impaired fat absorption, cystic fibrosis , other pancreatic exocrine disorders, bile secretion disorders, untreated celiac disease ;
- phase: ↓ calcium → ↑ parathyroid hormone → normalization of calcium, phosphaturia, stimulation of calcitriol formation → ↑ osteoclast activity → ↑ alkaline phosphatase ;
- phase: bone resorption (parathyroid hormone+calcitriol) → classic clinical symptoms of rickets and typical X-ray picture of the skeleton (craniotabes, delayed closure of the large fontanelle, caput quadratum, rachitic rosary, Harrison's furrow, pectus carinatum, genua valga, genua vara, delayed eruption of milk dentition , enamel defects, tooth decay);
- phase: depletion of calcitriol reserves, without which PTH cannot break down bone → ↓ calcium despite pronounced hyperparathyroidism → clinical symptoms of hypocalcemia (spasmophilia, tetany, laryngospasm, convulsions) and vitamin D deficiency (frequent and more serious ongoing respiratory infections);
- laboratory findings: Ca 2+ at the lower limit, then decreased, phosphate increased → normal → decreased, ALP high, parathyroid hormone increased, 25-OH-vitamin D decreased;
- treatment: vitamin D (cholecaciferol im eventual. po), calcium; with manifest tetany 10% calcium gluconicum iv
- vitamin D-dependent rickets type I – AR hereditary defect of renal 25-OH-D α-hydroxylase → blocked calcitriol synthesis → clinical manifestations of rickets in the 2nd trimester → lifelong calcitriol substitution;
- vitamin D-dependent rickets type II – AR hereditary receptor defect that causes resistance of target organs (gut and skeleton) to calcitriol → lifelong substitution of very high doses of calcitriol, difficult to treat;
- familial hypophosphatemic vitamin D-resistant rickets – X-linked disorder of reabsorption of phosphates in the proximal tubules of the kidneys → high losses of phosphates in the urine (“phosphate diabetes”) → manifestations after the start of walking: deformation of the lower limbs, growth retardation → substitution of phosphates and calcitriol.[1]
🔬 See Rickets Page for more information
Osteoporosis[edit | edit source]
- systemic metabolic disease of the skeleton, characterized by a disorder of the mechanical resistance of the bone, increasing the risk of fractures;
- diagnostic criteria in children: clinically significant history of fractures and abnormal densitometry (two-photon X-ray absorptiometry, peripheral quantitative computed tomography);
- primary osteoporosis (rare in children): osteogenesis imperfecta , idiopathic juvenile osteoporosis, etc.;
- secondary osteoporosis in oncological diseases ( leukemia treated with chemotherapy), systemic diseases with high-dose corticosteroid treatment ( JIA ), endogenous overproduction of cortisol ( Cushing's syndrome , Cushing's disease ) and neuromuscular diseases ( spina bifida , muscular dystrophy), anorexia nervosa , untreated celiac disease or immobilization;
- therapy: bisphosphonates;
- prevention: adequate physical activity and nutrition, vitamin D and calcium.[1]
🔬 See the Osteoporosis page for more detailed information
Familial disorders of calcium phosphate metabolism[edit | edit source]
- Familial hypocalciuric hypercalcemia (FHH) – mutation in the calcium receptor,
- neonatal hyperparathyroidism,
- hypercalciuric hypocalcemia,
- hereditary hypophosphatemic rickets.[3]
Links[edit | edit source]
Related Articles[edit | edit source]
Reference[edit | edit source]
- ↑ Jump up to: a b c d e f g LEBL, J, J JANDA and P POHUNEK, et al. Clinical Pediatrics. 1st edition. Galén, 2012. 698 pp. pp. 189-196. ISBN 978-80-7262-772-1 .
- ↑ Jump up to: a b SILBERNAGL, Stefan and Agamemnon DESPOPOULOS. Atlas of Human Physiology: 6th Edition, Completely Revised and Expanded. 3rd edition. Prague: Grada, 2004. pp. 290-293. ISBN 80-247-0630-X .
- ↑ ŽOFKOVÁ, I. Familial hypercalcemia and hypophosphatemia and their importance in the differential diagnosis of calcium-phosphate metabolism disorders [online]. ©2010. [feeling. 2011-04-17]. < https://www.prolekare.cz/casopysi/vnitrni-lekarstvi >.