Pelvis
The pelvis is formed by the union of the two pelvic bones and the sacral bone. It creates a limited space in which some abdominal organs are stored. It is a bone structure that shows significant sex differences (the female pelvis is adapted for childbirth).
Bone base[edit | edit source]
Os sacrum[edit | edit source]
It has the shape of a four-sided pyramid, basis ossis sacri turns cranially to the lower surface of the last lumbar vertebra, caudally directs apex ossis sacri and connects to the coccyx. The lateral sides form facies auriculares to connect with the hip bones.
The front surface (facies pelvina) is concave, four transverse lineae transversae run across it (at the point of fusion of the sacral vertebrae), on the sides there are four pairs of openings (foramina sacralia ventralia), through which the anterior branches of the sacral nerves emerge. The dorsal surface is convex, there is the foramina sacralia dorsalia for the exit of the posterior branches of the sacral nerves. In the middle of the dorsal side there is the canalis sacralis, which opens in the area of the apex as the hiatus canalis sacralis, where the last sacral and coccygeal nerves emerge.
Between the basis ossis sacri and the front surface, a rounded edge emerges (promontorium), from which the linea terminalis extends laterally, delimiting the entrance to small pans.
Os coxae[edit | edit source]
The pelvic bone is formed by the fusion of three paired bones (right and left) – the ilium, ischii and pubis.
- Os ilium
- Formed by the body (corpus) and the blade (ala ossis ilium). Cranially there is a well palpable crista iliaca, ventrally there is also a palpable spine (spina iliaca anterior superior), dorsally the spine is less prominent (spina iliaca posterior superior). Medially there is the facies auriculares to connect with the os sacrum. The inner surface is deepened in a flattened pit (fossa iliaca), which forms the bottom of the abdominal cavity. Caudally there is an arc-shaped linea arcuata (part of the linea terminalis). The outer surface of the shovel is covered by the gluteal muscles.
- Ischial axis
- It consists of a body (corpus), a shoulder (ramus ossis ischii) and a massive ischial hump (tuber ischiadicum). On the dorsal side, it extends into a sharp spine (spina ischiadica). The cranial part (pars pubica) is connected to the pubic bone and forms part of the boundary of the foramen obturatum.
- Os pubis
- Formed by the body (corpus) and the shoulder (ramus ossis pubis). Together with the ischial axis, it forms the boundary of the foramen obturatum. Medially there is a roughened surface (facies symphysis) to which the cartilage of the symphysis grows, connecting the two bones together. Above it we find a bump (tuberculum pubicum) from which extends a sharp edge (pecten ossis pubis).
Pelvic joint[edit | edit source]
On the dorsal side, the pelvic bones connect to the sacrum via the sacroiliac joint (SI joint), ventrally we find a connection via the symphysis, which connects the two pelvic bones in the area of the facies symphysis ossis pubis '.
Sacroiliac Joint[edit | edit source]
The Articulatio sacroiliaca connects the os coxae to the axial skeleton. This is a stiff joint (amphiarthrosis). The connection is ensured by strong ligaments. In the case of a woman at the end of pregnancy, their penetration occurs, which allows greater extensibility of the pelvis.
Symphysis pubica[edit | edit source]
Synchondrosis connecting the front part of the pelvic bones. The discus interpubicus, formed by a layer of fibrocartilage, is inserted between the joint surfaces. The posterior edge of the disc extends beyond the edge of the bones and arches as the eminentia retropubica (palpable per vaginam in women). Under normal circumstances, the connection is immobile. Hormonal (Relaxin) regulation at the end of pregnancy loosens the structure of the symphysis, allowing for expansion of the pelvis during childbirth.
Pelvic Dissection[edit | edit source]
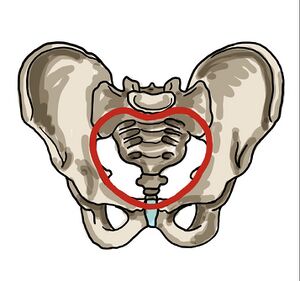
The pelvis is divided by the linea terminalis into a large (pelvis major) and a small pelvis (pelvis minor). It runs laterally from the promontory through the sacrum, then as the linea arcuata on the pelvic bone, to the eminentia iliopubica on the upper edge of the symphysis.
The pelvic region forms the abdominal floor. The small pelvis encloses the cylindrical space of the pelvic cavity. Cranially, it connects to the abdominal cavity in the area of the apertura pelvis superior, it opens caudally to the surface of the body as the apertura pelvis inferior.
Pelvic Planes[edit | edit source]
In order to evaluate the patency of the birth canal, the so-called pelvic planes were introduced, the size of which must correspond to the size of the newborn's skull in order to enable birth via the classical route. We distinguish four planes (craniocaudally): aditus (entrance), amplitudo (width), angustio (narrow), exitus (exit).
Aditus pelvis
- Aditus pelvis (entrance)
- The plane of the pelvic entrance (apertura pelvis superior), copies the course of the linea terminalis.
- In the direct direction, we determine the diameter recta (connector of the promontory and the upper edge of the symphysis), 11 cm, it is not possible to measure in clinical practice. Instead, we determine the diameter obstetrica (10.5 cm), per vaginam we measure the value of the conjugata diagonalis (the lower edge of the symphysis and the front edge of the promontory, approx. 12.5-13 cm) from which we subtract 2.5 cm. Transversally we determine the diameter transversa (the largest distance of the lineae terminales), 13 cm and in the oblique direction the diameter obliqua (connector of SI joint and eminence iliopubica), 12.5 cm.
- Amplitudo pelvis (width)
- Connects the S2–S3 interface with the center of both acetabulum and the center of the symphysis. Diameter recta (12 cm), diameter transversa ('12 cm) and diameter obliqua (13.5 cm ).
- Angustia pelvis (strait)
- Determined as the junction of the lower edge of the symphysis, spinae ischiadicae and the connection of the sacrum with the coccyx. We determine two directions, diameter recta (joint of lower symphysis and sacrococcygeal junction), about 11.5 cm' and diameter transversa (between the spinae), about 10 cm .
- Exitus pelvis (exit)
- Forms apertura pelvis inferior. It lies in the shape of a diamond between the end of the coccyx, the tubera ischiadica and the lower part of the symphysis. Here we determine the important dimension diameter recta (9.5 cm), during childbirth the coccyx is pushed away, thereby increasing the straight dimension (11-11.5 cm), and will allow the passage of the fetus through the birth canal.
Pelvic tilt[edit | edit source]
We determine standing. Basic parameters of pelvic inclination: inclinatio pelvis superior (conjugata anatomica makes an angle of 60° with the horizontal), inclinatio pelvis inferior (the joint between the tip of the coccyx and the lower edge of the symphysis forms an angle of 10°) and the angle formed by the pelvic plane with the horizontal (30°).
The tilt of the pelvis affects the position of the abdominal organs while standing and walking, which does not exert their full weight on the pelvic floor. During pregnancy, the growing uterus pushes the abdominal organs towards the spine, which is thus more loaded. Subsequently, compensatory hyperlordosis occurs in the lumbar region.
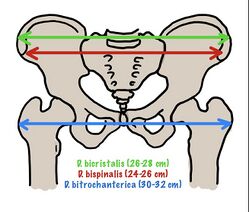
Measuring pelvic dimensions[edit | edit source]
External pelvic dimensions[edit | edit source]
In the prenatal clinic, we measure the pelvis from the outside using a pelvimeter (according to Baudelocque–Breisky). We measure in the position on the back, side and on the gynecological table.
- Distantia bispinalis - distance of spinae ilacae ant. vulture. (25–26 cm).
- Distantia bicristalis - the greatest distance between the ridges of the hip blades (28-29 cm).
- Distantia bitrochanterica - the distance between the two major trochanters (31–32 cm).
- Conjugata externa (diameter Baudelocque) – the distance between the top of Michaelis root (thorn L5) and the upper edge of the symphysis (19-20 cm).
Internal pelvic dimensions[edit | edit source]
The approximate value of the direct diameter of the pelvic entrance is obtained by subtracting 9 cm from the measured value of the conjugata externa. Another measurable value is diameter transversa exitus pelvis (the distance of the ischial tubera). We perform the measurement on the gynecological table, using a crossed pelvimeter. Add 1.5 cm (soft tissue) to the measured value. The usual value is around 11 cm. The distance can also be estimated using Rubešek's touch (the fist of the right hand is pressed between the tubercle, if it does not fit, it indicates a transverse narrowing of the pelvis).
The length of the conjugata diagonalis can be determined by internal examination. We introduce the pinched 2nd and 3rd fingers into the sheath, with the third finger we try to reach the promontory, while the radial edge of the hand rests on the symphysis (we mark the place of contact on the finger and then measure). The normal distance is 13 cm. Values around 12 cm mean a borderline narrowing of the pelvis, which can be linked to complications during childbirth, values around 11 cm mean a significant narrowing of the pelvis, which can make a natural birth impossible, usually indicated for caesarean section.===Pelvic tilt measurement===
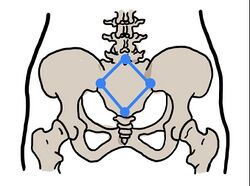
In clinical practice, we evaluate the pelvic inclination by determining the Michaelis route on the dorsal side of the pelvis. It is a rhombus formed by the union of the structures of the spinae iliacae posteriores superiores, the sacrococcygeal junction and the spine of the L5 vertebra. In a standing woman, this structure is usually visible as skin pits above the individual structures. The longitudinal axis of the route measures about 11 cm, the transverse (about 10 cm). The course of the transverse axis intersects the longitudinal axis and divides it into a cranial (4 cm) and a caudal (7 cm) section. The link between the L5 mandrel and the spins should be about 6.5 cm.
A symmetrical Michaelis root indicates the correct shape of the pelvis. Deviations in the shape of the root are a risk factor for cephalopelvic disproportion. If asymmetry is detected, the birth is considered risky and a caesarean section is often indicated.
Pelvic gender differences[edit | edit source]
Gender differences in the shape of the bony pelvis are very pronounced. The shape of the female pelvis is hormonally modified during puberty and represents a significant secondary sexual characteristic. Adjusting the shape of the female pelvis is necessary for the creation of birth canals, which must correspond to the physiological dimensions of the newborn skull.
Overall, the female pelvis is wider (more spacious) and lower than the male pelvis. The lower arm of the pubic bones in women converge at an obtuse angle (arcus pubicus) while in men they converge at a sharper angle (angulus pubicus). In women, the lower arm of the pubic bone is usually slender and smoothly curved, in the male pelvis we observe a sudden curvature in the place of the crista phallica.
The Promontorium protrudes less in the female so that the entrance to the pelvis is transversely oval, in the male it protrudes and forms a heart-shaped pelvis. Incisura ischiadica major on the female pelvis is formed by a regular arch, wider and shallowly cut, on the male pelvis the upper edge of the incision is clearly deeper. The distance from the center of the fossa acetabuli to the upper edge of the facies symphysis and the lower edge of the tuber ischiadicum are roughly the same in men, while in women the distance to the tuber ischiadicum is significantly smaller than the facies symphysialis.
The symphysis pubica of the female pelvis is lower (4.5 cm) than that of the male pelvis (5 cm), at the end of pregnancy it loosens and allows for a slight expansion of the birth canal. The coccyx is shorter and more mobile in women, it bends backwards during the passage of the fetus and thus increases the space of the birth canal (about 2.5 cm).
Types of female pelvis gynaecooid (40%), android (20%), anthropoid (25%), and platypellloid (5%) as per Caldwell Molley classification of female pelvis helps to assess cephalopelvic disproportion in slow progress of labour to choose the safe mode of delivery as individualised intrapartum care.
Topographical anatomy of male pelvis[edit | edit source]
Muscles of the Male Pelvic Floor[edit | edit source]
The male pelvic floor muscles are dome-shaped structure functions as hammock. It has three layers: deep, middle, and superficial arranged in a complex relationship with the surrounding bony pelvis, ligaments, fascia and nerves.
The muscles of the superficial layer are bulbospongiosus, ischiocavernosus, superficial transverse perineal and external anal sphincter. Their clinical significance is their involvement in ejaculation, urinary and faecal continence. The middle layer consists of perineal membrane, the deep transverse perineal, the sphincter urethrae and the compressor urethrae which are accountable for urinary continence during increased intra-abdominal pressure like jumping/coughing/sneezing/climbing.
The muscles of the deep layer are the levator ani, iliococcygeus, ischiococcygeus and pubourethralis. These act as pelvic diaphragm for pelvic organs' support towards continence. The levator ani is formed by puborectalis, pubococcygeus, and iliococcygeus. Around the rectum the puborectalis forms a U-shaped sling and aids in faecal continence.
The pudendal nerve arises from S2-4 of sacral plexus with three main branches such as the inferior rectal nerve, perineal nerve and the dorsal nerve of the penis innervating the penis, the bulbospongiosus and ischiocavernosus muscles, perineum, anus, external anal sphincter, and urethral sphincter. The sensory role of pudendal nerve are external genital sensation, bowel and bladder continence, orgasm and ejaculation.
Links[edit | edit source]
Related Articles[edit | edit source]
References[edit | edit source]
- BENEŠ, George. Study Materials [online]. ©2009. [cit. 2010]. <http://jirben.wz.cz>.
- ŠIHÁK, Radomír – GRIM, Miloš. Anatomy. 2nd, edit. and add edition. Prague : Grada Publishing, 2002. 470 pp. vol. 2. ISBN 80-7169-970-5.
- HÁJEK, Zdeněk – CZECH, Eugene – MARSHAL, Karel. Obstetrics. 3. edition. Prague : Grada, 2014. 538 pp. ISBN 978-80-247-4529-9.