Birth traumatism
From WikiLectures
Neonatal trauma can occur during pregnancy, during childbirth, in the postnatal period or in connection with iatrogenic impairment. Macrosomia, cephalopelvic disproportion, protracted labor are among the predispositions for birth injuries in newborns.[1]
- Soft tissue injuries: caput succedaneum, cephalhematoma, subgaleal bleeding, conjunctival and retinal bleeding, sternocleidomastoid muscle injuries, abrasions, lacerations, cuts, ear injuries, peripheral nerve injuries (facial nerves, brachial plexus, ...).
- Skull injury: fissure, fracture, impressive fractures.
- CNS injury: epidural haemorrhage, subdural haemorrhage, subarachnoid haemorrhage, intraspinal haemorrhage, spinal cord injury, tractional spinal cord injury, haemorrhage under tentorium cerebelli.
- Long bone injuries: fracture of the clavicle, humerus, femur, epiphysiolysis.
- Intra-abdominal injury: subcapsular hematoma of the liver, rupture of the spleen, bleeding into the adrenal gland.
Risk periods:[edit | edit source]
- early after birth,
- 48 hours after birth,
- 4-5 day after birth.
A traumatized newborn should be hospitalized/observed at the JIRP[2].
Risk factors:[edit | edit source]
- unripe fetus,
- breech birth,
- operative/instrumental delivery,
- delivery of a large fetus or cephalopelvic disproportion,
- precipitous birth,
- binding labor → arm dystocia, uterine dystocia,
- abnormal fetal position,
- Congenital developmental defects [2].
Head and neck injuries[edit | edit source]
Petechiae, ecchymoses[edit | edit source]
- Petechiae, ecchymoses are most often found on the head, less often on the neck and chest.
- Neonatal thrombocytopenia must be ruled out with a larger seeding.
- Petechiae usually get absorbed within 3 days.
- Hemorrhages under the conjunctiva may also occur with more severe facial involvement, which will also heal without treatment within 2 weeks.
- in the case of more widespread subconjunctival bleeding an examination of the fundus can be recommended to rule out retinal hemorrhages [1].
Obstetric tumor (caput succedaneum)[edit | edit source]
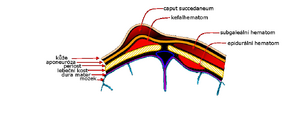
Diagram of head soft tissue injuries: birth tumor, cephalhematoma, subgaleal hematoma and epidural hematoma
Template:See Caput succedaneum for more details
- Diffuse percolation of the leading tissues of the head during childbirth
- The swelling is localized between the galea aponeurotica and the skin, we can observe petechiae or small hematomas on the skin.
- The swelling overlaps the cranial sutures.
- Treatment is not indicated, it resorbs within a few days[1].
Cephalhematoma[edit | edit source]
Template:More detailed information can be found on the Kefalhematoma page
- It is a subperiosteal hemorrhage, limited to the surface of one bone without accompanying changes in the skin.
- Most often above the parietal bone.
- Usually restricted by cranial sutures.
- It increases within a few hours after birth, in 5% it is caused by a linear fracture of the skull (does not require treatment), exceptionally there is also a fracture with an impression or intracranial bleeding - in the case of extensive KFH (mainly after forceps births) – we consider ultrasound or X-ray of the skull.
- Fluctuation is palpable.
- Can calcify within 3 weeks.
- For larger KFH, it is good to monitor the blood count (danger of anemia) and bilirubin levels (risk of jaundice from extravasal breakdown of erythrocytes).
- Treatment – usually not necessary, it resorbs spontaneously within a few weeks/months[2].
- puncture, evacuation or drainage are contraindicated due to the risk of infection.
- Rarely, calcification and hyperostosis can occur - it is usually temporary [1].
Subgaleal hematoma[edit | edit source]
- This is bleeding under the aponeurosis.
- It exceeds the border of the skull bones, blood loss can be significant and lead to anemia and hyperbilirubinemia.[3]
- Clinical picture - general swelling of the head with hematoma around the ears and eyes.
Skull fractures[edit | edit source]
- Subperiosteal fractures → subperiosteal bleeding.
- Linear fractures - occur after forceps delivery and usually do not require therapy.
- Impressive lbi fracture – the "ping pong ball" phenomenon, with an impression > 0.5 cm a neurosurgical solution is necessary.
Fractures of the mandible, nasal cartilage[edit | edit source]
Fracture of the clavicle[edit | edit source]
- It is the most common perinatal fracture ever.
- It is detected soon after birth - by palpation as a crepitation above the umbilicus.
- Sometimes swelling of the soft tissues and limited movement of the limb is also noticeable.
- But it can only be detected after the release of 7th-10th day, until after the formation of the muscle.
- It is not necessary to perform x-rays.
- Treatment - it is recommended only to examine the HK and fix it when the child is at rest (sleeping).
- Fixation – flexion of the elbow up to 90°, abduction of the arm up to 60° (the so-called "pinning by the shirt sleeve").
- Callus is formed on the 7th-10th. day, then fixation is no longer necessary.
- The prognosis is excellent, it heals without consequences[1].
Intracranial stroke[edit | edit source]
Traumatic epidural, subdural, or subarachnoid hemorrhage[edit | edit source]
- It occurs in case of cephalopelvic disproportion, prolonged or forceps birth.
- A large subdural hemorrhage associated with a rupture of the tentorium cerebelli or falx cerebri is rare —if massive, it can rapidly lead to the death of the newborn.
Intracranial hemorrhage after vacuum extraction[edit | edit source]
- Subgaleal haemorrhage, scalp laceration, cephalhematoma,
- Acute subdural hematoma (hemophilia A).
Intrauterine subdural hematoma[edit | edit source]
- The cause is usually intrauterine trauma, coagulopathy, macrocephaly.
- Occurrence supratentorial × infratentorial × both.
- Often coincident with hydrocephalus[2].
Cerebral venous thrombosis[edit | edit source]
- It is a multifactorial disease.
- Perinatal risks for the mother are infections, vasculitis, malignancies, autoimmunity, metabolic diseases, prothrombotic pharmacotherapy.
- Perinatal risks in newborns are congenital thrombotic conditions (Leiden mutation f. V,protein C and S deficiency).
- As a differential diagnosis, we must consider this disease in all intracerebral and intraventricular perinatal cerebrovascular accidents[2].
Eye injuries[edit | edit source]
Subconjunctival and retinal hemorrhages[edit | edit source]
- In the case of subconjunctival bleeding, it is always necessary to examine the fundus of the eye, as we often also find retinal hemorrhages - this is a benign finding, but the examination is important especially from a forensic point of view.
- They arise most often as a result of a sharp rise in intrathoracic pressure[2].
Blockage of the nasolacrimal duct[edit | edit source]
Facial nerve paresis[edit | edit source]
- Peripheral paresis n. VII.
- Peripheral paresis of this nerve can occur after delivery by forceps in the area of the foramen stylomastoideum or as a result of local pressure on the facial nerve.
- The prognosis depends on whether the nerve was damaged only by compression or whether the nerve fibers were severed.
- More common than central.
- Clinical picture : weak paralysis of the entire face, including the eyelids – lagophthalmos (hare's eye - lagos = hare).
- On the affected side, the eyelid is permanently open, the corner is drooping, when crying there is a typical asymmetric cry (the mouth is pulled towards the healthy side).
- Central paresis n. VII
- Caused by bleeding into the CNS.
- Clinical picture : spastic paralysis of half to 2/3 of one side of the face (opposite to where the bleeding is).
- Diff. dg – hypoplasia or agenesis of the depressor anguli oris muscle, …
- Therapy – non-specific - in peripheral palsy, protection of the cornea.
- Improvement in mobility usually occurs spontaneously within 7–10 days (with the subsidence of edema)[1].
Injury of the sternocleidomastoid muscle[edit | edit source]
- The cause is muscle aplasia/hypoplasia, dystrophy, hematoma, abnormal position of the uterus, traumatic birth.
- Torticollis
- Torticollis is a twisting of the head to one side caused by ischemia or bleeding in the sternocleidomastoid muscle, contracture or shortening of the muscle.
- Sometimes there is a palpable fibroma on its surface.
- Timely rehabilitation led by a pediatric neurologist is important to avoid permanent muscle shortening and skull deformities[1].
- Therapy: positioning, rehabilitation, rarely operative correction.
Extremity injuries[edit | edit source]
Paresis of the brachial plexus[edit | edit source]
- According to the Mallet score, we distinguish permanent × transient.
- Often during the delivery of large fetuses in connection with brachial dystocia.
- Upper type ( Duchenne-Erb ) – more common (about 90% of brachial plexus paresis).
- It is an injury in the range of C5–C6, usually due to compression by swelling or bleeding, less often there is a disruption of the nerves.
- Abduction and external rotation of the shoulder is missing → UE hangs weakly - there is typical adduction and internal rotation of the shoulder.
- Grasp Reflex can be performed.
- When C4 is affected at the same time, paresis of the phrenic nerve occurs with unilateral paresis of the diaphragm.
- Therapy: loose fixation, rehabilitation according to Vojta (but only on the 2nd-4th day).
- Lower type (Klumpke's) – less common.
- Injury in the C7–C8 range.
- The distal part of the UE is affected → "pinch fingers".
- Hand often livid (bluish).
- If Th 1 is affected at the same time, the cervical sympathetic system will be affected – we can develop Horner's syndrome (ipsilateral miosis, ptosis of the eyelid and enophthalmos).
- Therapy – the limb should be at rest for the first 7-10 days, then we will start rehabilitation.
- The aim is to prevent the occurrence of contractures.
- Treatment should be conducted by a pediatric neurologist.
- Prognosis - depends on the degree of disability.
- Improvement may occur within a few weeks (after swelling or bleeding has disappeared).
- The majority recovers within 3-6 months, in 92% we find a normal finding at 1 year of age[1].
Humerus injury[edit | edit source]
Femur injury[edit | edit source]
- Transverse complete fractures × subperiosteal fractures[2].
Injury to the internal organs[edit | edit source]
Subcutaneous fat necrosis[edit | edit source]
- It occurs during childbirth due to impaired blood circulation in places of increased pressure (shoulders, buttocks).
- Necrotic foci appear during the 1st week of life, are irregularly defined, hard, slightly above the skin level, white to reddish, 1-10 cm in size.
- Treatment is not necessary, within 6-8 weeks the deposits soften and disappear spontaneously.
Liver rupture[edit | edit source]
- Liver injury is the most common intraparenchymal injury.
- Predisposition is fetal macrosomia, intrauterine asphyxia, prematurity, hepatomegaly and hemocoagulation disorders.
- A subcapsular hematoma can tamponade further bleeding and the child appears normal for the first 24–48 hours.
- Nonspecific symptoms are tachycardia, tachypnea, anemia.
- Early ultrasound diagnosis reduces mortality[2].
Rupture of the spleen[edit | edit source]
- It has a similar clinical picture to liver rupture.
Adrenal bleeding[edit | edit source]
- Predisposition is trauma, stress, hypoxia, associated infection.
- The diagnosis is verified by ultrasound.
Perforation of the colon[edit | edit source]
- Due to obstruction, trauma, diverticulum, iatrogenic etiology.
Testicular torsion[edit | edit source]
- Prenatal × postnatal.
Diagnosis of CNS damage[edit | edit source]
- Clinical diagnostics;
- laboratory diagnostics (Acid-base balance, Blood count + diff., coagulation, biochemistry including S–lactate);
- imaging methods;
- Transfontanellar CNS ultrasound;
- CT including contrast (detects bone integrity damage, subacute and chronic subdural hematoma);
- MRI, MRI angio (evidence of ischemia, thrombosis);
- Electroencephalography, polygraphy[2].
Clinical manifestations of a traumatized newborn[edit | edit source]
- CNS: behavioral disorders, neurological abnormalities (irritability, convulsions, hypotonia, apathy, lateralization of reflexes);
- circulatory disorders (pallor, acrocyanosis, thermolability);
- respiratory disorders (Respiratory distress syndrome, apnea);
- circulatory disorder (systemic hypotension, vasomotor disturbances, shock);
- MODS (Disseminated intravascular coagulation, renal failure, liver failure, …);
- manifestations of pain.
Links[edit | edit source]
Related Articles[edit | edit source]
External links[edit | edit source]
- JEŽOVÁ, Marta – HOTÁRKOVÁ, Sylva – MŮČKOVÁ, Katarína, et al. Hypertext Atlas of Neonatal Pathology : Multimedia support for teaching clinical and health disciplines [online]. Portal of the Faculty of Medicine of Masaryk University [online], ©2010. The last revision 27.9.2011, [cit. 26.11.2011]. <http://portal.med.muni.cz/clanek-527-hypertextovy-atlas-novorozenecke-patologie.html>.
Source[edit | edit source]
- BENEŠ, Jiří. Study materials [online]. ©2007. [cit. 2009]. <http://www.jirben.wz.cz/>.
- Havránek, Jiří – Traumatic newborn
References[edit | edit source]
- ↑ a b c d e f g h HRODEK, Otto – VAVŘINEC, Jan, et al. Pediatrics. 1. edition. Prague : Galén, 2002. 72-74 pp. ISBN 80-7262-178-5.
- ↑ a b c d e f g h i HAVRÁNEK, J.: Traumatic newborn
- ↑ DORT, Jiří. Neonatology : selected chapters for students of the Faculty of Medicine. 1. edition. Prague : Karolinum, 2005. ISBN 80-246-0790-5.
