Tumors of the liver and subhepatic landscape
Tumors of the liver and the subhepatic landscape are mainly linked by the proximity of their localization, the resulting symptomatology and often unfavorable prognosis. Tumors of the subhepatic region include biliary tract tumors, gallbladder and pancreatic head.
Tumors of the liver
We understand liver tumors as tumors
- primary (benign and malignant) and
- secondary (metastases - mainly from the GIT).
Benign tumors
Pathological classification
Depending on the tissue from which liver tumors originate, they are divided into epithelial, mesenchymal, and mixed. Epithelial tumors:
- hepatocellular - nodular transformation, focal nodular hyperplasia, hepatocellular adenoma,
- cholangiocellular - gallbladder adenoma, biliary cystadenoma.
- Mesenchymal tumors
Tumors arising from the interstitium and perivascular tissues belong to this group:
- Mixed tumors
- mesenchymal hamartoma,
- benign teratoma.
Focal nodulation of hyperplasia
It is difficult to distinguish from malignancy (macroscopically and microscopically). It is formed by an accumulation of hepatocytes, Kupffer cells and small bile ducts with congested fibrous septa. It occurs 2-8 times more often in women, between the ages of 20 and 50. a year. The probability of occurrence during puberty and pregnancy increases significantly. It is therefore associated with hormonal influences and the use of hormonal contraception.
Clinical picture'
- does not manifest, usually discovered by chance,
- 80% do not exceed the size of 5 cm,
- larger ones can appear as other tumors.
Diagnosis
- ultrasound, CT and scintigraphy are used for diagnosis. biopsy to confirm.
Therapy
- for small tumors, the treatment is conservative (monitored), in the case of an unclear diagnosis, resection of part of the liver is indicated.
Therapies'
- hemangioma is one of the tumors that we usually only monitor,
- if it would lead to complications, we treat:
- res=== Liver adenoma ===
Liver adenoma, or hepatocellular adenoma, is also associated with the use of oral contraceptives, and affects mainly women aged 30-40 years. In 30%, it perforates and hemorrhages. It can turn malignant, it is a pre-cancer (possibility of malignancy 10%)!
Therapies'
- removal is indicated, as the lethality is up to 20% in case of spontaneous perforation with bleeding.
Hemangioma
Thanks to USG, today we diagnose it much more often, mainly in people aged 30-60 years, more often in women. The size varies between 4-30 cm. Ruptures are rare. It usually didn't cause the wearer any trouble before being revealed. A biopsy is never performed, there is a risk of massive bleeding.
ection for tumors over 4 cm,
- for minor embolizations of supply and drain vessels (interventional radiology).

|
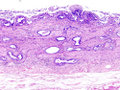
Ultrasound: liver hemangioma |
Malignant tumors
We divide them into 'primary and secondary. These include hepatocellular carcinoma, fibrolamellar carcinoma, cholangiocarcinoma, hepatoblastoma, mesenchymal malignancies (angiosarcoma, fibrosarcoma) and others (carcinoid, ...).
Hepatocellular carcinoma
Hepatocellular carcinoma (HCC) is the most common primary malignant liver tumor. [1] Worldwide, hepatocellular carcinoma is the fifth most common cancer in men and the eighth in women.[2] The development of this cancer most often occurs in patients with chronic liver disease, usually in the field of cirrhosis of various etiologies (alcohol abuse, chronic hepatitis B and hepatitis C). Worldwide, hepatocellular carcinoma is the third most common oncological cause of death. [3] In our population, it is among the less common tumors with an incidence of 5-7/100 000 inhabitants'.[2] The only potentially curative therapy is surgical treatment (resection or transplantation) .
Fibrolamellar Carcinoma
Highly differentiated hepatocellular carcinoma. It is difficult to distinguish from adenoma and nodular hyperplasia. It usually mounts to cirrhosis. It is 75% resectable, so it has a better prognosis.
Cholangiogenic carcinoma
It affects the intrahepatic bile ducts. It rarely manifests as inflammation of the bile ducts. It is more common in primary sclerosing cholangitis. The main manifestation is jaundice. The prognosis is often poor, the tumor is only discovered when it is unresectable.
Liver metastases
Metastases cause up to 90% of liver malignancies. 20% are metastases from stomach cancer, 25% from colon, 50% metastases from pancreatic cancer. For solitary and innumerable (up to 3) anatomic and non-anatomical resection is indicated (mainly for colorectal cancer).
Therapy of liver tumors
Conservative
It is mainly performed for metastases from colorectal cancer and breast cancer, unless cirrhosis is significant:
- cholecystectomy (toxic cholecystitis prophylaxis), a. gastroduodenalis probing and catheter insertion,
- discontinuation of contraception or estrogen preparations in adenoma, if the adenoma does not regress → surgery,
- multiple liver metastases are treated with a local intra-arterial CHT (via a. hepatica) subcutaneously implanted port-system for 14 days, the treatment has only a minimal systemic effect.
Surgical
Surgical treatment is indicated for benign tumors (adenomas, bleeding tumors or large hemangiomas) and some malignant ones. The tumor must be limited to one lobe (T1–T3).
Surgery is the only treatment option, only 20% of patients are curatively operable (late onset of symptoms). We use the following approaches:
- transverse or median laparotomy, or an incision along the arch,
- hemihepatectomy – oriented in the line of vena cava – gallbladder,
- extended hemihepatectomy on the right - according to the ligamentum falciforme hepatis,
- resection of the liver lobe on the left - left lobe up to the lig. falciform,
- peripheral resection.
Liver metastases: Peripheral resection without orientation according to anatomical structures. Ultima ratio indicates liver transplantation in hepatocellular carcinoma, if it has not yet metastasized.
Tumors of the subhepatic landscape
Gallbladder carcinoma
It is a relatively rare malignancy that affects more of the female population, with median incidence of about 73 years.
Etiology
Higher risk with cholelithiasis or calcified gallbladder, clear RF – ulcerative colitis (9-21 times higher risk). Other – primary sclerosing cholangitis, congenital duct anomalies and parasitic infections.
Clinical picture
Early stages are asymptomatic. Advanced stages have symptoms like other (benign) gallbladder diseases - pain in the right lower jaw, nausea, fatty diet intolerance, anorexia, weight loss and jaundice.
Physical finding
The most common sign of cancer is icterus. We can feel resistance in the right lower jaw, hepatomegaly, ascites may also be found. Non-specific symptoms - pain in the lower jaw, weight loss, pruritus, fever.
Diagnosis
Most are diagnosed at an advanced stage, the main detection methods are CT and US. ERCP is good for localizing biliary obstruction. cholangiocarcinoma can be diagnosed earlier than gallbladder cancer, due to obstruction and jaundice.
many cholangiocarcinomas are considered to be metastatic adenocarcinomas with unknown primary localization.
Histopathology
Adenocarcinomomas account for 85 % and squamous cell or mixed cancers for15 %. Rare – adenosquamous ca, leiomyosarcoma or mucoepidermoid ca.
Bile duct tumors account for 90% of adenocarcinomas.
Treatment
in 1–2 % we find cholecystectomy carcinoma (without previous diagnosis).
Surgical treatment
Surgical treatment is the basic treatment method of early stages, of the proximally located tumors, about 15–20 % are resectable, out of distally located up to 70 %. Resectability is assessed by CT or MRI. For the unresectable, it is important to palliatively bypass the obstruction (bypass, stent). Postoperatively, local recurrences are common - in gallbladder cancer up to 85 %, in bile ducts up to 25–40 %.
Radiotherapy
Radiotherapy can have a palliative effect, brachyradiotherapy is sometimes used in bile duct cancer
There is no evidence of efficacy of adjuvant radiotherapy or radiochemotherapy.
Chemotherapy
Chemotherapy is also used palliatively, mainly 5-FU.
Prognosis
- In the early stages, after a cholecystectomy, the 5-year survival rate is 80%,
- in growth, 5-year survival after surgery is 30%, in nodular involvement 15%,
- median survival after palliative care is 6 months.
Bile duct tumors
Benign tumors
- Rare,
- papillomas, polyps - the essence is fibromas, lipomas, granulomas; …,
- they can become obstructive and need to be removed.
Malignant tumors
- It is most often a medullary carcinoma.
- They infiltrate the bile duct or are in the papilla (it is difficult to decide whether they come from the bile duct, duodenum or pancreatic duct).
- Unfortunately, it is worse in the upper parts - they are often diagnosed late (Klatskin's tumor).
- Clinical image – intermittent painless obstructive icterus/jaundice with loss of appetite, weight loss.
- Therapy:
- papillary tumor - hemiduodenopancreatectomy;
- tumors of the strain:
- resection and anastomosis of the bile duct into the GIT;
- but more often palliative - choledochoduodenoanastomoses.
Carcinoma of the head of the pancreas
Pancreatic head carcinoma is an adenocarcinoma arising from the duct epithelium of the exocrine part of the pancreas. Because of its location, it typically manifests itself in obstructive jaundice (compression of the bile ducts), pancreatic insufficiency (obstruction of the pancreatic duct), dyspepsia, epigastric pain (sometimes shooting into the back). The prognosis of the disease is not good. The only curative therapy is resection. But this is often not possible, because the tumor is detected late, palliative procedures are performed. Chemotherapy and radiotherapy are not effective.
Links
Related Articles
- Diagnostic imaging methods in the examination of the pancreas, liver and spleen
- Diagnostic imaging methods in the examination of the gallbladder and bile ducts
Source
- BENEŠ, Jiří. Studijní materiály [online]. [cit. 5.5.2010]. <http://jirben.wz.cz>.
References
- ČEŠKA, Richard, et al. Interna. 1. edition. Prgue : Triton, 2010. 855 pp. ISBN 978-80-7387-423-0.
Recommended literature
- ZAVORAL, Miroslav, et al. Pancreatic cancer. 1. edition. Prague : Galén, 2005. 287 pp. ISBN 80-7262-348-6.
- EVANS, Douglas Brian, et al. Pancreatic cancer. 1. edition. New York : Springer, 2002. 423 pp. ISBN 0-387-95185-7.
- FURUKAWA, Toru. , et al. Molecular targeting therapy for pancreatic cancer: current knowledge and perspectives from bench to bedside. Journal of Gastroenterology [online]. 2008, vol. 43, p. 905-911, Available from <https://link.springer.com/article/10.1007%2Fs00535-008-2226-1>. DOI: 10.1007/s00535-008-2226-1.
- CARTWRIGHT, Thomas. Cancer of the Pancreas: Are We Making Progress? A Review of Studies in the US Oncology Research Network. Cancer Control [online]. 2008, vol. 15, p. 308-311, Available from <http://www.moffitt.org/CCJRoot/v15n4/pdf/308.pdf>. ISSN 1073-2748.
- ↑ POVÝŠIL, Ctibor – ŠTEINER, Ivo – DUŠEK, Pavel, et al. Special Pathology : interaction of harmful substances with living organisms, their mechanisms, manifestations and consequences. 2. edition. Prague : Galen, 2007. 430 pp. pp. 209-210. ISBN 978-807262-494-2.
- ↑ Jump up to: a b BRŮHA, Radan. Hepatocellular carcinoma [online]. ©2012. [cit. 2015-11-03]. <https://web.archive.org/web/20160331222721/http://zdravi.e15.cz/clanek/postgradualni-medicina/hepatocelularni-karcinom-466724>.
- ↑ CICALESE, Luca. Hepatocellular carcinoma [online]. ©2015. [cit. 2015-11-03]. <https://emedicine.medscape.com/article/197319-overview>.