Viral hepatitis
Hepatitis is an inflammatory disease of liver tissue of viral origin. Different types of this disease include hepatitis A - G, TTV.[1] HBV is a DNA virus, the others are RNA viruses.
With all types of hepatitis, the infection can be of varying intensity: it often occurs inapparently, abortively (briefly, influenza or dyspeptic syndrom). Viral hepatitis can be acute or chronic (duration of the disease over 6 months). The typical (symptomatic) form is icteric, however, generally, the anicteric form is more common.
Hepatitis should be considered with any liver disease, the cause and severity of liver disease should be determined. During viral hepatitis, the prodromal stage, the stage of liver damage and the stage of convalescence should be monitored. The infection can also lead to asymptomatic carriers.
Histological evaluation includes grading (the intensity of inflammatory changes - infiltration)and staging (the progression of fibrosis).
The cholestatic form resembles obstructive jaundice, which can make the diagnosis difficult. The malignant or fulminant form is characterised by liver failure, high mortality. The stage of liver damage lasts for 2-8 weeks, if there is no improvement, we refer to this condition as prolonged course, which can become chronic.
During the convalescence period, functional disorders of the gastrointestinal tract are common (loss of appetite, intolerance to fatty foods, etc.), often also posthepatic hepalgia (pain in the liver region - caused by adhesions between the liver capsule, diaphragm and peritoneum).
Diagnostics[edit | edit source]
- Serology - determination of viral antigens and antibodies in serum (EIA);
- Molecular genetic testing - determination of viral nucleic acid in serum (PCR, hybridisation);
- liver biopsy – evaluates grading and staging, does not identify the causative agent, indicated in chronic hepatitis, not acute;
- Biochemistry – the first biochemical change in VH is the increase in transaminases – in prodromal stage (with acute VH, ALT increases more than AST), bilirubin.
| hepatitis | antigen |
|---|---|
| HAV | anti–HAV |
| HBV | HBsAg, HBeAg, anti–HBc, HBV DNA |
| HCV | anti–HCV, HCV RNA |
Transmission[edit | edit source]
- By feces orally - A, E (acute only)
- By blood, or sexual intercourse - B, C, D, G (acute or chronic)
Symptoms[edit | edit source]
- Prodromal stage - fatigue, weakness, loss of appetite, joint pain;
- Symptomatic stage - hepatic jaundice (↑ indirect bilirubin, bilirubin and urobilinogen in urine, dark urine, hypocholic stool), dyspepsia, epigastric pain, hepatomegalia.
Complications[edit | edit source]
- Fulminant hepatitis (liver failure, encefalopathy);
- liver cirhosis;
- hepatocellular carcinoma
Differential diagnosis of hepatitis[edit | edit source]
Anamnesis[edit | edit source]
As part of the family history, we focus on the occurrence of diseases of liver, bile ducts, familial hyperbilirubinemia and hemolytic conditions. We determine the same in the personal history of the patient as well as diseases that could affect the course of VH -diabetes, immunodeficiency, surgeries, blood transfusions. Epidemiological anamnesis is also important - we are looking for contact with the infection, other infections in the patient’s surroundings, vaccinations, the possibility of infection by sexual intercourse, stay in nature (harmful water sources,…). For the pharmacological history, we specifically ask about the use of contraception and hormonal preparations, antidepressants, analgetics. The history of substance abuse is crucial.
ALT Dynamics[edit | edit source]
- The highest values of transferases occur in viral hepatitis (prodromal stage - 2x, increased up to 50x after two weeks, they normalise around week 8).
- It is characterised by a rapid rise (approximately 30x) - toxic liver damage.
- In drug and alcohol intoxications, there is a slight increase.
Therapy of viral hepatitis[edit | edit source]
The basis of the therapy is rest and diet. The treatment of acute hepatitis is symptomatic and supportive, except in VHC, where early treatment with interferon may prevent the transition to chronicity. The patients leave the Infectious Diseases Department after jaundice disappears and the transferases fall below 3x the norm, followed by a check-up at hepatology.
Hepatitis A[edit | edit source]
__ The causative agent is HAV, which is an RNA virus from the Picornaviridae family (Enteroviridae, Enterovirus 72), that has a direct cytolytic effect. HAV is a small virus (27-30nm), genetically homogenous, resistant to the external environment. It is an exclusively human pathogen.[2] It spreads by the faecal-oral route (“dirty hand disease”), often by contaminated food and water, rarely parenterally. The entrance gate is the digestive tract and it is excreted in faeces. Transplacental transmission is not possible.[3]
The virus is highly resistant to external influences. It is excreted in faeces as early as 2 weeks before the onset of symptoms and continues for about a week (up to 2 weeks)[3] after the symptoms stop. The patient is the most contagious before the end of the incubation period.
The course of infection[edit | edit source]
The incubation period is 15-48 days.[3] First, the prodromal (“preicteric”) stage begins (dyspepsia, fatigue, fever, weight loss). This is followed by the symptomatic stage (“icteric”) - the leading symptoms are jaundice, dark urine and acholic stool. The course is milder and shorter than in VHB. Cholestatic symptoms are rare and may occur fulminantly. HAV does not cause chronic infections.[2]
Diagnostics[edit | edit source]
- Detection of antibodies
Diagnostics is done using anti-HAV antibodies. We perform the examination of specific IgM in serum (anti-HAV-IgM), the increase in transaminases and bilirubin and the slight increase in ALP. Negative test in immunocompetent individuals excludes infection. IgM persists in serum for 3-6 months after infection, IgG persists long-term. The infection leaves a long-term to lifelong immunity. The main diagnostic marker.
- Electron-microscopic detection of virus in faeces [2]
It can be detected in the second half of the incubation period and shortly after the onset of clinical symptoms.
- Detection of antigen and RNA [2]
In stool, similar to microscopy.
Therapy[edit | edit source]
Treatment is symptomatic - rest, no alcohol, a diet with carbohydrates (possibly glucose) and fat reduction. Corticosteroids only in fulminant forms.
Complications[edit | edit source]
The severity of the infection increases with age (90% are asymptomatic in young children). In 10%, it is a prolonged form, which, however, does not lead to chronicity. Chronic infection and carriers do not exist.
Complications: fulminant liver failure (rare), myocarditis, encephalopathy, cryoglobulinemia, bone marrow hypoplasia, spleen rupture, pancreatitis, Guillain-Barré syndrome.[3]
Prevention[edit | edit source]
Vaccination with an attenuated vaccine increased health surveillance at the site of the outbreak. By clinical examination and liver function monitoring, new cases of infections are identified. Immunolactively administered immunoglobulin (NORGA) is administered to the exposed.
Hepatitis B[edit | edit source]
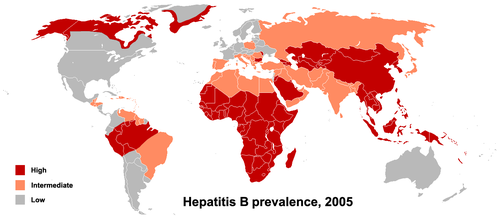
__ The causative agent is HBV, which is a DNA virus (Hepadnaviridae). Hepatocytes are broken down by the cytotoxic action of T and NK cells (they recognize the virus antigen bound to the surface of the hepatocyte). The virus is carried by 5% of the population. It is one of the most serious viral diseases in humans – one in five carriers dies of cirrhosis, one in nine from hepatocellular carcinoma. It is transmitted through blood and bodily fluids (sexual transmission). The incubation period is 30-180 days (most often 60-90 days)[4].
- Antigens
- HBsAg (surface, Australian Ag) - 3 subtypes. It allows the virus to penetrate the hepatocyte. Its detection is a sign of the presence of the virus in the body (at any period of infection, in acute and chronic hepatitis - in the replication and integration phase).
- HBcAg (core antigen) - a protein that envelops the DNA of the virus. Present on the hepatocyte membrane (immunofluorescence in biopsy), where it is exposed to MHC I and recognized by TC and NK cells. Can be identified only in the period of replication (acute and chronic replication phase).
- HBeAg (envelope antigen) - part of HBcAg, which is secreted only during viral replication (in so-called wild type viruses), mutants that do not form HBeAg do exist. The antigen indicates active virus replication in the liver cell (in acute and chronic replication hepatitis). It is a sign of high infectivity of the patient.
- Antibodies
- Anti-HBs – neutralizing (by binding to HBsAg on the surface of the virus prevents its entry into the cell), it is in the serum of people who have had HBV infection (then anti-HBc and anti-HBe are also present), or in people vaccinated ( isolated anti-HBs positivity).
- Anti-HBc – the most specific and sensitive antibody in HBV infection - is present after any exposure to the virus (it is a trace that the virus leaves behind in the body).
- Anti-HBe – is usually present after the infection (not in the period of active replication of the virus, when HBeAg predominates).
In the serum of infected persons or persons after infection, either the relevant antigen or antibody is detected, always one which is in excess and not bound in the immunocomplexes.
| HBsAg | anti-HBs | HBeAg | anti-HBe | IgG anti-HBc | IgM anti-HBc | HBV DNA | |
|---|---|---|---|---|---|---|---|
| Acute VH B | + | – | + | – | + | + | + |
| Chronic VH B-active replication | + | – | + | – | + | +/– | + |
| Chronic VH B-inactive carrier | + | – | – | + | + | – | – |
| Past infection | – | + | – | + | + | – | – |
| Successful vaccination | – | + | – | – | – | – | – |
Thus, in the period of active inflammation (acute hepatitis B and chronic hepatitis in the replication phase), HBsAg and HBV DNA (PCR) are detected as signs of the presence of virus and anti-HBc (with the presence of HBcAg in the hepatocyte membrane) and HBeAg. HBV DNA is not detectable in an inactive carrier, there are no HBcAg in the hepatocyte membrane, therefore no HBeAg is detected (however, there are anti-HBc and anti-HBe antibodies) - HBeAg seroconversion - anti-HBe. After infection, only antibodies are detected, not antigens (seroconversion HBsAg - anti-HBs, HBeAg - anti-HBe).
Etiopathogenesis[edit | edit source]
Hepadnavirus, has reverse transcriptase. Its genome is a partial double helix of circular DNA.
The genome is unique, each piece of DNA encodes something (even more than one thing).
- HBcAg ("core") - a nucleocapsid protein, it still has a part of the DNA called pre-core, when it is translated in its entirety (pre-core + core), HBeAg is formed.
- HBsAg ("surface") - is put on the membrane of hepatocytes, it is on the envelope of the virus and much of this antigen is produced by the hepatocytes and freely released into the circulation.
- DNA polymerase – reverse transcriptase, occupies most of the genome.
- HBX - a protein from the X region, is essential for viral replication, acts as a transcriptional transactivator of viral genes, and also as a transactivator of many host promoters. It is thought to play a role in the development of hepatocellular ca.
The course of infection[edit | edit source]
It often occurs inapparently, especially in children and immunodeficient patients.
- Acute infections
Elimination by the immune system in 85-90% of the cases. The virus enters the liver through the bloodstream. Through HBsAg, it enters the cell, where it replicates in the nuclei of hepatocytes. HBsAg and HBeAg are released into the serum. HBcAg is bound to the cell surface, which is recognized by immunocompetent cells that induce lysis of affected hepatocytes. Release of virions into the circulation and attack of other hepatocytes, the release of enzymes (transaminases - increase of ALT and AST in serum), decreased ability of the liver to secrete bilirubin (hyperbilirubinemia to hepatocellular jaundice). In case of an excessive immune response, fulminant hepatitis with acute liver failure.
- Chronic stage
10-15%. Depending on the success of the immune response, two situations occur. Replication - constant inflammatory activity (multiplication of the virus with HBcAg on the surface of hepatocytes, which are lysed by lymphocytes) - can progress to liver cirrhosis to cancer. At this stage the patient is highly infectious, JT levels are elevated. Furthermore, integration - decrease in inflammatory activity (stopping the multiplication of the virus, HBcAg disappears from the hepatocyte membrane, viral DNA integrates into the hepatocyte genome) - so-called carrier, infectivity is less but not zero, liver tests (transaminases) are normalized.
During perinatal transmission, due to the immature immune system, the child always develops chronic infection with the risk of developing carcinoma after the age of 20. It must be vaccinated passively after birth (applies to all newborns of HBsAg positive mothers), actively vaccinated after one week, and only then can the mother breastfeed the baby.
Acute hepatitis B[edit | edit source]
The prodromal stage lasts up to several weeks, and arthralgia or rash often occurs. Jaundice lasts longer than in the case of the VHA. Arthralgia and pruritic rash due to circulating immunocomplexes may be present. The worst complication is the development of liver failure - especially in the elderly and exhausted.
90% of neonates, 30–40% of children, 5–10% of adults lead to chronicity. Fulminant form - in about 1 in 1,000, mostly women, the patient dies within 10 days of hepatic coma caused by very rapid destruction of hepatocytes by cytotoxic T lymphocytes.
Chronic hepatitis B[edit | edit source]
It manifests itself either as a consequence of the acute or primarily - without an obvious acute phase.
Histologically we distinguish:
- benign form - persistent hepatitis (patient has mild clinical difficulties, slightly elevated liver tests, not infectious);
- progressive form - aggressive hepatitis (the patient has significant clinical difficulties, impaired liver function, has HBsAg and HBeAg in the blood, but lacks antibodies, the virus multiplies and is in the blood, the course and prognosis are serious, the risk of cirrhosis and hepatocellular carcinoma, is infectious).
According to the activity of the virus, we distinguish:
- replication phase - multiplies in hepatocytes;
- integrated phase - latent storage in the genome.
During replication, various mutants of the virus are created:
- pre-core mutant - does not form HBe antigen - more often liver failure, faster cirrhosis, less sensitive to interferon;
- then only the defective mutant is selected during treatment, starting treatment as soon as possible before the mutant is formed.
Asymptomatic carrier of VHB[edit | edit source]
They have no clinical, biochemical or biopsy symptoms. Only the presence of HBsAg in the serum is evident. It may disappear spontaneously, rarely it may develop into chronic VHB. Therefore, if such a patient emerges, they are dispensarized. We detect HBeAg and anti-HBe to detect active virus replication, we detect ALT.
Pregnancy hazard - 90% risk of infecting a baby during childbirth, therefore HBsAg examination is performed on all pregnant women. In the case of positivity, the newborn must be passively immunized within 12 hours.
Diagnostics[edit | edit source]
Prior to the development of jaundice, transferases are elevated. Serology is performed by ELISA. As the first sign of infection, HBsAg appears in the serum (a few weeks before the others), which disappears from the serum during recovery. When HBs cannot be detected (in small amounts of HBV), we detect IgM against HBc. Examination of the replication or integrated phase of chronic HBV is an antigen - HBe and IgM against it indicate a replication phase.
If HBeAg disappears, the patient's infectivity decreases. There is an increase in viral DNA polymerase in serum. Anti-HBc remains for life and are markers of past infection. Anti-HBs occur during acute infection, but mainly after vaccination. The most sensitive marker of infection is PCR.
Therapy[edit | edit source]
- IFN-α (necessity of s.c. application, for so-called pegylated IFNs once a week is enough);
- lamivudine (viral DNA synthesis blocker, p.o application);
- adefovir dipivoxil (indicated for lamivudine resistance).
Treatment is indicated for chronic infection (over 6 months) and viremia over 100,000 copies/ml.
Immunisation[edit | edit source]
The principle is the binding of the antibody to HBsAg, which aims to prevent the virus from penetrating the hepatocyte:
- active (prophylactic) - administration of an immunogenic fragment of HBsAg leading to the formation of anti-HBs;
- passive (post-exposure) - administration of anti-HBs from the serum of immunized donors.
Hepatitis C[edit | edit source]
__
The causative agent is the HCV-RNA virus (Flaviviridae). We differentiate its genotypes and their subtypes, the virus is easily subject to mutations. There are 6 types of viruses and a large number of subtypes (genotype 1b occurs most often in the Czech Republic). Spread parenterally (blood derivatives – haemophiliacs, i.v. drug addiction, hemodialysis, sexual transmission, perinatally from mother to fetus, transplant grafts), it is about 100 times less contagious than VH
Acute HCV has an ICD code of B171, chronic B182.
The course of infection[edit | edit source]
The incubation period is 15–160 (most often around 50) days[5].
- Acute infection (asymptomatic or icteric form), in 15% spontaneous elimination, in 85–90% it becomes chronic;
- chronic infection.
The infection is often asymptomatic, or it takes the form of vague dyspeptic problems. It is usually without jaundice. It may manifest itself clinically after years as liver cirrhosis (or its complications) or hepatocellular carcinoma. Jaundice occurs more often in the elderly. Hepatic failure is rare. The development of liver cirrhosis is slow, accelerated by HBV and alcohol. Asymptomatic carriers are rare.
Diagnostics[edit | edit source]
We determine serologically - anti-HCV antibodies (not only in infected persons but also in those who eliminated the virus spontaneously or by antiviral treatment). PCR detection of viral RNA is an indicator of active infection. The rise in Anti-HCV is seen about 3 weeks after exposure, it has no preventive effect against reinfection. It is characterized by a small link between biochemistry and histology (even slightly increased ALT, large changes). For this reason, we have to resort to liver biopsy more often.
Ig production may be delayed; if acute HCV is suspected, the test should be repeated. Chronic hepatitis C requires a biopsy with staging (advanced liver fibrosis) to show a risk of progression to liver cirrhosis. The virus cannot be grown on tissue cultures, so PCR or Ig anti-HCV is detected.
Treatment[edit | edit source]
At the moment (2020) the treatment consists of directly acting antivirals (DAA) in interferon-free mode, and often in ribavirin-free mode. This prevents serious side effects of pegylated interferon (PEG-IF alpha) and ribavirin.
Genotyping of the virus is important before starting.
Treatment has minimal side effects.
Efficiency is close to 100 %.
Drugs block the multiplication of the virus in the hepatocyte. According to the place of operation, we divide them into 3 groups of antivirals :
- viral protease blockers, cleaving viral proteins
- NS5A replication complex inhibitors (assembling viral particles)
- viral polymerase inhibitors
Efficacy is assessed in 12 and 24 weeks after the end of therapy.
2 Negative HCV PCR tests performed 12 weeks apart indicate the elimination of the virus from the body (the patient achieved a so-called sustained virological response).
DAA: Directly Acting Antivirals (Most Important Fixed Combinations)
Genotype specific:
Sofosbuvir (400 mg) + ledipasvir (90 mg): 1-0-0, standard 12 weeks. Treatment for genotypes 1 and 4.
Grazoprevir (100 mg) + elbasvir (50 mg): 1-0-0, standard 12 weeks. Treatment intended for genotypes 1 and 4 (in the Czech Republic only for 1a and 1b with low viremia).
Pangenotypes:
Sofosbuvir (400 mg) + velpatasvir (100 mg): 1-0-0, standard 12 weeks. Treatment for HCV genotypes (1-6).
Glecaprevir (100 mg) + pibrentasvir (40 mg): 3-0-0, standard 8-12 / 16 weeks. Treatment for HCV genotypes (1-6).
Sofosbuvir (400 mg) + velpatasvir (100 mg) + voxilaprevir (100 mg): 1-0-0, standard 8-12 weeks. Treatment for HCV genotypes (1-6).
This treatment may or may not be combined with Ribavirin (according to the genotype of the virus, severity: liver cirrhosis) and the therapy lasts for a maximum of 12 weeks. The side effects are quite mild but the treatment is very expensive (the price is still falling).
Unlike previous therapy, there is a success rate of up to 97%.
The ultimum refugium is then a liver transplant.
Prophylaxis[edit | edit source]
There is no effective vaccine against HCV (due to the high variability of the virus). Reduction of the risk of infection: in health care, in high-risk populations ( MSM ).
Screening examinations of at-risk individuals.
Hepatitis D[edit | edit source]
__
The causative agent is defective RNA virus delta (HDV), which is not capable of independent replication, it requires enzymatic equipment of HBV.
These are either:
- co-infection with HBV + HDV,
- superinfection of HDV in primarily infected by HBV (more dangerous).
It can be fulminant hepatitis, other times the development of liver cirrhosis.
Clinical picture[edit | edit source]
The incubation period is 2-7 weeks. Superinfection leads to deterioration of liver function - failure or faster liver cirrhosis. During co-infection, the course is usually better.
Diagnostics[edit | edit source]
Detection of specific antibodies against delta antigen is performed by ELISA.
Hepatitis E[edit | edit source]
__
Originator[edit | edit source]
The causative agent is an RNA virus from the family Hepeviridae (formerly Caliciviridae)[6]. It is resistant to the external environment and has several genotypes[2]:
- Genotype 1 in Asia and Africa - epidemic,
- genotype 2 in Africa,
- genotype 3 (USA) and 4 (China) also in pigs; may have the character of a zoonosis and cause sporadic cases in humans (including in Europe),
- genotype 5 and 6 in feral pigs,
- genotype 7 and 8 in camels.
Epidemiology[edit | edit source]
A rare infection occurs in developing countries with insufficient levels of safe water supply - in Central and East Asia, Africa (and the Mediterranean), Central America. In the Czech Republic, it appears not only as an imported infection. Cases of transfusion transmission are also described.
Clinical picture[edit | edit source]
The virus is transmitted by the faecal-oral route. Clinically, it is similar to HAV, but the course is more severe - jaundice is more pronounced, failure is more frequent. In the immunocompetent, it is acute, it becomes chronic only in the immunosuppressed. It is very dangerous in pregnancy when lethality during the infection in the 3rd trimester reaches up to 20 %[7]. In the rest of the population, lethality is between 0,5 and 4 %[7].
Diagnostics[edit | edit source]
By demonstration of anti-HEV and detection of IgG and IgM antibodies. Detection of RNA virus in faeces or blood is possible at the end of the incubation period. It is not fully known whether the infection leaves long-term immunity[2].
Hepatitis F[edit | edit source]
__
- The causative agent is a virus similar to VHB,
- the possibility of oral transmission is also being considered.
| This article is a stub. You can join the authors and edit it. You can discuss the changes at discussion. |
Hepatitis G[edit | edit source]
__
- The causative agent is a VHC-like virus;
- parenteral transmission, diagnosis of HGV RNA, detection of anti-HGV rather indicates an infection, often combined with VHB or VHC;
- most infections are asymptomatic, but fulminant hepatitis can occur, chronic infections are characterized by the absence of significant histological impairment of liver tissue;
- it turns chronic, but clinical, morphological and laboratory signs of liver disease are not present even after decades of infection. Therefore, therapy, prevention or other interventions are not indicated.
- the positive effect of VHG infection on HIV infection is being considered.
TTV virus infection[edit | edit source]
- DNA virus transmitted parenterally and faecally-orally;
- only viral DNA can be detected, not an antibody response;
- is similar to HGV (combination with HBV or HCV, both acute and chronic infection).
Other viruses associated with hepatitis[edit | edit source]
- CMV,
- EBV,
- HSV,
- adenovirus,
- enterovirus.
Links[edit | edit source]
Related articles[edit | edit source]
Bibliography[edit | edit source]
- ↑ MUDr. Stanislav Plíšek, Ph.D.,MUDr. Jan Galský, CSc.,Společnost infekčního lékařství ČLS JEP, Česká lékařská společnost Jana Evangelisty Purkyně,<http://www.cls.cz/dokumenty2/resitele/r016.rtf>
- ↑ Jump up to: a b c d e f
ŽAMPACHOVÁ, Eva. Downloadable lectures and materials from dr. Žampachová [online]. [cit. 2012-01-12]. <http://mujweb.cz/zampach/motol/?redirected=1521314685>.
Cite error: Invalid
<ref>tag; name "zampachova" defined multiple times with different content - ↑ Jump up to: a b c d MUNTAU, Ania Carolina. Pediatrie. 4. edition. Prague : Grada, 2009. pp. 393-394. ISBN 978-80-247-2525-3.
- ↑ Doporučené postupy pro praktické lékaře. Virové hepatitidy. 2001. reg. č. o/020/016. Autoři: Stanislav PLÍŠEK a GALSKÝ Jan. Available from <http://www.cls.cz/dokumenty2/postupy/r016.rtf>.
- ↑ Doporučené postupy pro praktické lékaře. Virové hepatitidy. 2001. reg. č. o/020/016. Autoři: Stanislav PLÍŠEK a GALSKÝ Jan. Available from <http://www.cls.cz/dokumenty2/postupy/r016.rtf>.
- ↑ International Committee on Taxonomy of Viruses (ICTV). Virus Taxonomy: 2009 Release [online]. The last revision 2009-xx-xx, [cit. 2012-01-14]. <https://talk.ictvonline.org/taxonomy/>.
- ↑ Jump up to: a b WHO. Hepatitis E [online]. The last revision 2005-01-xx, [cit. 2012-01-14]. <http://www.who.int/?ReturnUrl=http%3a%2f%2fwww.who.int%2fen%2fnews-room%2ffact-sheets%2fdetail%2fhepatitis-e>.
Sources[edit | edit source]
- PASTOR, Jan. Langenbeck's medical web page [online]. [cit. 2010]. <http://www.freewebs.com/langenbeck/Gastroenterologie.rar>.
- BENEŠ, Jiří. Studijní materiály [online]. [cit. 2010]. <http://jirben2.chytrak.cz/materialy/infekceJB.doc>.
- HAVLÍK, Jiří, et al. Infektologie. 2. edition. Praha : Avicenum, 1990. pp. 393. ISBN 80-201-0062-8.
- LOBOVSKÁ, Alena. Infekční nemoci. 1. edition. Praha : Karolinum, 2001. pp. 263. ISBN 80-246-0116-8.