Viral infections of the nervous system: Difference between revisions
Pokornaade (talk | contribs) No edit summary |
Pokornaade (talk | contribs) No edit summary |
||
| Line 42: | Line 42: | ||
=== [[Rabies|Rabies (rabies, lyssa)]] === | === [[Rabies|Rabies (rabies, lyssa)]] === | ||
[[File:Rabies patient.jpg|thumb|300px|Patient with rabies ]] | [[File:Rabies patient.jpg|thumb|300px|Patient with rabies ]] | ||
''' | '''Rabies''' (lyssa) is a [[viruses|viral]] infectious disease that spreads from wild and domestic animals. Once clinical symptoms break out, the disease is always fatal. | ||
The Czech Republic has been considered "'''Rabies-free'''" since 2004 (rabies does not occur in the Czech Republic). In the Czech Republic, you can find imported rabies or rabies after a bat bite. There is an increased risk of rabies at the borders with Poland and Slovakia (these countries are not "Rabies-free"). | |||
==== Patogeneze ==== | ==== Patogeneze ==== | ||
[[ | [[File:Rabies negri bodies brain.jpg|thumb|300px|Characteristic Negri bodies in Purkinje cells of the cerebellum in a patient who died of rabies]] | ||
* Primární [[encefalitida]] způsobená ''[[Lyssavirus|lyssavirem]]'', patřící do skupiny Rhabdoviridae, | * Primární [[encefalitida]] způsobená ''[[Lyssavirus|lyssavirem]]'', patřící do skupiny Rhabdoviridae, | ||
* přenáší se slinami zvířete při pokousání či infikovaným škrábnutím, | * přenáší se slinami zvířete při pokousání či infikovaným škrábnutím, | ||
Revision as of 16:34, 13 February 2022
CNS viral infections usually occur within generalized viruses. Multiple nerve structures are often damaged at the same time.
- gateway of viral infection: respiratory tract, gastrointestinal tract, urogenital tract, skin
- the infection spreads to the CNS along the peripheral nerves / hematogenously
- involvement: meninges → meningitis, brain and spinal cord tissues → encephalitis or myelitis, anterior horns → poliomyelitis, sensitive spinal ganglia of spinal cord → radiculitis
- acute to chronic infections, the virus can survive in nervous structures for years asymptomatically, a number of virosis seasonal occurrence
- immunosuppression and cytostatics create the conditions for virus replication
- active immunization (today eg rare polioviruses)
- diagnosis: detection of virus from cerebrospinal fluid, faeces, nasopharynx, increase in antibody titer in fluid or blood
- treatment of most viruses only symptomatic, exception: herpes viruses - aciclovir
- antiviral sera are available for some diseases, active immunizations are given for others [1]
Viral meningitis
Viral meningitis is the most common viral infection of the CNS along with inflammation of the soft envelope of the brain (leptomeningitis). Aseptic meningitis includes, in addition to viral meningitis, other forms of meningitis where culture does not reveal the causative agent. The incidence of viral meningitis is difficult to monitor, but it is reported to affect about 1 in 3000 patients with viremia .[2]
Etiology
The most common causative agents are
- enteroviruses - currently more than 85% of cases),
- mumps virus,
- HSV 2,
- EBV,
- rarely lymphocytic choriomeningitis, AIDS.
Pathogenesis
The viral pathogen can enter the CNS in 2 ways: hematogenously (most common) and neurogenically (typical of herpesviruses)[2];
- In the spring period, young patients are affected by mumps virus; parotitis can be complicated by meningitis, there is also a possibility of residual hearing loss;
- mononucleosis is caused by EBV, affects adolescents, may be complicated by serous meningitis, monocytosis in the blood count, increased fatigue lasting several months!;
- enteroviral infections (caused by ECHO viruses) occur seasonally in adolescents in the summer and autumn, spread by the fecal-oral route, mainly affect the children under one year of age, more common in lower social groups;
- Coxsackie viruses cause C-viruses with severe muscle pain;
- HSV 2 is responsible for 5% of viral meningitis, ¼ of these patients have primary genital infection;
- lymphocytic choriomeningitis is spread by airborne transmission from rodent feces;
- HIV infection is thought of in high-risk groups; HIV antibodies appear 1-3 months after the onset of illness.
Clinical signs
- 1) Prodromal phase (flu) - fever, muscle and throat pain, diarrhoea, exanthema, fatigue and malaise; lasts 3-7 days
- Latency phase - 2-5 days with virtually no difficulties
- 2) Neuroinfection phase - photophobia, headache, nausea to vomiting, dizziness, meningeal symptoms, somnolence;
- recovery usually within 2 weeks;
- some cases may proceed asymptomatically or only through the first phase.
Pathological-anatomical pattern
- Inflammation causes edema, engorgement of the meninges and their infiltration by lymphocytes;
- it also affects the surface of the brain (spinal cord).
Differential diagnosis
- Subacute onset distinguishes a group of clinically severe meningitis;
- Tuberculous and mycotic meningitis, leptospirosis, sarcoidosis, meningocarcinomatosis, partially treated bacterial meningitis;
- the mild, easy course and spontaneous recovery of acute meningitis differs from the severe course and prognosis of these subacute and chronic meningitis.
Auxiliary examinations
- CSF from Lumbar puncture fluid: proteinocytological association, predominance of lymphocytes over monocytes, mild proteinorachia;
- Virus culture from: CSF (early collection), nasal swab, throat swab, stool;
- rise in serological titres in the acute phase of the virus compared to convalescence;
- sedimentation usually normal, leukocytosis at most mild;
- the course of the disease mild;
- virus identification fails in about 20-40%.[3]
Treatment
- Symptomatic and supportive with rest and vitamin supplementation;
- acyclovir i.v. - when HSV type 1 or 2 is detected;
- prognosis is always good (self-limiting disease with complete recovery in 7-10 days).
Viral encephalitis
They occur most in the tropics. Viruses affect the brain in 4 ways:
- directly (acute encephalitis or meningoencephalitis)
- after various latencies ("slow" viral encephalitis)
- indirectly via the immune system (allergic, post-infectious or post-vaccination encephalomyelitis)
- encephalopathy (Reye's syndrome) also develops within the viral infection
Acute viral encephalitis
The result of acute viral encephalitis are neuronal and glia defects occurring with inflammation and edema.
Etiology
- Mumps, HSV, VZV, EBV.
- Substantial link to the vector: tick – tick encephalitis, Russian spring encephalitis; mosquito - western equine disease (USA), western Nile encephalitis (Africa).
- Post-infectious encephalitis – follow childhood infections (measles, chickenpox, rubella), it is not a direct effect of the virus.
Clinical manifestations
- General manifestations ("influenza"): muscle pain, fever, headache, meningeal reactions, cerebrospinal fluid cell proliferation.
- Symptoms of brain impairment - focal/diffuse, according to location.
- With hemisphere involvement → epilepsy, involuntary movements, paresis, confusion, speech disorders.
- Rhombencephalits = defects in cerebellar and brainstem structures.
- Mesencephalic defect→ oculomotoric and autonomic disorders.
- Cerebellar defect→ ataxia, dysarthria.
- Brainstem defect → nystagmus, quadruparesis, cranial nerve palsy.
- Spinal cord defect→ mixed motor, sensitive and autonomic dysfunction.
Prognosis
- Usually lasts for several weeks;
- the prognosis depends on the type of virus;
- mortality HSV infection 20-30%, in mumps only 2%;[4]
- also the neurological consequences vary in severity.
Tick-borne encephalitis
Tick-borne encephalitis (TBE) is a disease caused by the tick-borne encephalitis virus (TBEV), which is an arbovirus. The disease can lead to meningitis, meningoencephalitis, and severe encephalomyelitis. The course is variable- from abortive forms (with few symptoms) to a typically two-phase course with central nervous system involvement. The clinical picture manifests as a febrile illness with headaches and neurological symptoms. There is no specific antiviral therapy: the treatment is only symptomatic. TBE mortality is low, but permanent neurological sequelae are relatively common. It is possible to vaccinate against TBE.
TBEV is one of the most common causes of aseptic neuroinfections in the Czech Republic. The clinical picture of meningitis prevails in children with up to 2/3 of children showing cognitive deficits after having KME and have memory problems.
Epidemiology
Tick-borne encephalitis is an endemic local seasonal neuroinfection.
- Originator: arbovirus (arthropod-borne virus, enveloped RNA virus) of the family Flaviviridae.
- Infection reservoir: small rodents and larger forest animals, sheep, goats.
- Transmission (vector): by sucking blood of infected nymphs or adult ticks (Ixodes ricinus)
- the virus is in the saliva of ticks, so a short suction time is enough to transmit the virus.
- the virus survives in the salivary glands of the tick and in the tick there is also a transovarian transmission of the virus
- rarely, transmission is via the alimentary route- by consuming unpasteurized milk from infected goats and sheep.
- Incubation period: 3-28 days.
The reported incidence of tick-borne encephalitis in the Czech Republic in the years 2000–2009 is 500–1000 cases per year, i.e., 5-10 patients per 100,000 population per year. It has been known in the Czech Republic only since 1945 and its occurrence is most frequent in the Vltava, Berounka, and Sázava river basins, in Central and Southern Bohemia, most often from April to October.
Clinical symptoms and course
The incubation period of the disease is 7–14 days, with an extreme variation of the duration of symptoms (3–30 days). Most infections are inapparent. After 1-3 weeks of incubation, a two-phase course is usually typical:
- Phase 1 ("flulike") – Viremia with headache and muscle pain, fever, fatigue. The condition improves in a few days. An apparent recovery in the form of an afebrile period (2-7 days) follows. The asymptomatic period that lasts 1–20 days.
- Phase 2 – meningeal symptoms: headache, photophobia, encephalomyelitic symptoms: alterations of consciousness (sleepiness to coma), cranial nerve disorders, bulbar syndrome, weak limb paresis, high fever, sleep disturbance, vomiting, and tremors.
Based on the predominant disability, we can divide encephalitis into several forms:
- inapparent (specific antibody production only)
- abortifacient (nonspecific symptoms similar to influenza illness)
- meningeal (viral meningitis)
- encephalic (gray and white brain disease with neurological symptoms)
- encephalomyelitic (involvement of gray, white matter and anterior horns); weak paresis, especially of the brachial plexus as segments C5–7 are most often affected by the process.
- bulbocervical (involvement of the medulla oblongata), bulbocervical forms can also lead to the failure of vital centers and thus to death.
Diagnosis
- positive meningeal symptoms in people living in the endemic area;
- a history of a typical two-phase course;
- tick bite data - indicates only a part of patients with TBE;
- detection of specific antibodies from serum - ELISA with detection of early IgM antibodies, IgG class antibodies are formed very quickly, for which their avidity can be determined
- other serological methods: specific virus neutralization test, rise of specific antibodies
- cerebrospinal fluid examination: aseptic inflammation with a leukocyte count ranging from 100-200 leukocytes/μL, slightly elevated protein levels
- EEG in the acute phase: diffuse pathological recording with a predominance of slow waves.
Treatment
So far it is only symptomatic (analgesics , antiemetics , antipyretics). Resting is especially important. Relieving lumbar puncture can be performed (tens to hundreds of lymphocytes in the CSF, slightly higher protein). We treat paresis by administering vit. B and rehabilitation. Anti-edematous treatment (mannitol) and corticoids also have a positive effect. It is recommended to avoid the sun, prolonged television and higher mental strain.
Prevention
Vaccination with an inactivated virus vaccine (FSME-IMMUN (Baxter) approved since 1976 and Encepur (Novartis) approved since 1991). The basic vaccination schedule consists of 3 doses. Vaccines are well tolerated, the most common adverse reactions being a fever in the range of 38.0-39.0 °C (20% of children; most often in the age group of 1-3 years; most in the period from February to March, i.e., in the period of frequent respiratory infections), injection site pain and, rarely, muscle weakness. The World Health Organization recommends vaccination against tick-borne encephalitis to all people living in the endemic area, including children.
The disease prevention includes regimens including appropriate clothing covering the entire body, the use of repellents, early removal of the tick and disinfection of the injection site.
Drinking of pasteurized milk is also a prevention (it is also spread by the milk of infected animals, including cow's milk).
Prognosis and consequences
More severe forms have convalescent period lasting weeks to months. Residual symptoms persist (in 10% of patients) in the form of peripheral weak paresis, and memory, concentration, and sleep disorders.
Herpetic meningoencephalitis
- HSV typ I – herpes labialis et oralis – encefalitis.
- HSV typ II – herpes genitalis –serous meningitis in newborns.
Etiology
- Herpes DNA viruses include: HSV types I and II, VZV, EBV, CMV;
- capable of long-term latent survival in nervous tissue with the possibility of exacerbation infection;
- transmission throughout the year in all age groups - by contact, by air;
- HSV type I
causes severe hemorrhagic-necrotic encephalitis selectively affecting the frontotemporal area, 30% mortality
- HSV typ II
- causes serous meningitis - like other viral meningitis.
Pathological-anatomical picture
- Necrotizing encephalitis (necrosis most often in the cortex of the frontal lobes);
- brain severely swollen at autopsy, sanguineous meninges;
- intranuclear eosinophilic inclusion bodies;
- biopsy shows antigen herpes simplex by immunofluorescence and positive culture within 48 hours.
Clinical picture
- Non-specific headaches and fever - progress in a few days to seizures with impaired consciousness, focal symptoms correspond selectively to the lower parts of the frontal and temporal lobes;
- olfactory hallucinations, partial seizures with complex symptomatology, behavioral changes;
- involvement of the dominant hemisphere - aphasia - one of the main symptoms;
- cerebral edema can cause death (tentorial herniation);
- survival associated with memory defect.
Diagnosis
- In the acute phase brain biopsy;
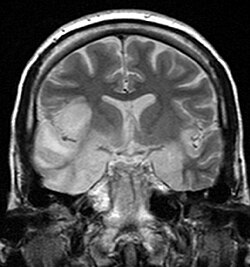
- after initiating treatment a non-specific positive CT or MRI finding is sufficient;
- at first, normal CT will show frontotemporal hypodensity (necrosis);
- cerebrospinal fluid - multiplication of lymphocytes, higher protein;
- EEG - generalised slowdown with periodic discharges temporally
Diferential diagnostics and therapy
- Dif. dg.: other encephalitis, brain abcess, tumor; jiné encephalitidy, absces mozku, tumor;
- Unlike other viral CNS infections, we have a causal drug - aciclovir.
- aciclovir should always be used immediately if a herpes etiology of encephalitis is suspected, till proven othervise
Links
Similar articles
References
- BENEŠ, Jiří, et al. Infekční lékařství. 1. vydání. Galén, 2009. 651 s. s. 179, 527-528. ISBN 978-80-7262-644-1.
- ↑ SEIDL, Zdeněk a Jiří OBENBERGER. Neurologie pro studium i praxi. 1. vydání. Praha : Grada Publishing, 2004. ISBN 80-247-0623-7.
- ↑ Skočit nahoru k: a b POVÝŠIL, Ctibor a Ivo ŠTEINER, et al. Speciální patologie. 2. vydání. Praha : Galén-Karolinum, 2007. s. 297-299. ISBN 978-80-7262-494-2.
Source
Herpetic meningoencephalitis is one of the most serious meningoencephalitis in children and adults. Even with the possibility of causal therapy, the diagnosis is often delayed, the disease has a high mortality and the survivors have a high percentage of permanent neurological consequences.
Etiopatogenesis
Etiology
Human herpesvirus is a DNA virus that includes two important strains:
- Human herpesvirus 1 (HHV-1), known as herpes simplex virus 1 (HSV-1), which causes herpes gingivostomatitis that responds to antiviral therapy but even without treatment, is a self-limited disease. In addition to local infections, HSV-1 and HSV-2 are the cause of severe encephalitis. It is more common in adulthood.
- Human herpesvirus 2 (HHV-2), known as herpes simplex virus 2 (HSV-2), causes genital lesions. It is the cause of neonatal encephalitis associated with maternal genital infection.
- HHV transmission: saliva, genital secretions, blood and vertically. The gateway is most often the respiratory tract, damaged skin and genital mucosa. The virus can also enter the macroorganism intravenously or transplacentally.
- In HSV-1, in primary infections are most common: primary gingivostomatitis, pharyngitis, keratoconjunctivitis and encephalitis.
- When the virus is reactivated in herpes labialis in immunosuppressed patients these things may occur: herpetic stomatitis or even esophagitis or even dissemination to generalization of infection.
- In HSV-2, we encounter neonatal encephalitis and genital herpes.
However, HSV-1 can cause diseases more typical of HSV-2 and vice versa.
HSV primarily affects the medial temporal cortex as well as the frontal and parietal lobes.
Pathogenesis of the encefalitis
- It is not sufficiently clarified in humans.
- In animal models, the virus is thought to pass to the CNS through peripheral nerves. Virus-induced apoptosis may then play a role in the molecular pathogenesis of the disease.
- Encephalitis mainly affects the temporal lobes (60%), separate extratemporal involvement is observed in about 15% of patients.
- In children, herpetic encephalitis is often a manifestation of herpetic primary infection (approximately 80% of children do not have a history of labial herpes). In neonates, the infection occurs during the passage through the birth canal, with a higher risk of infection when the mother acquired herpes during pregnancy. Mothers with pre-existing and recurrent genital herpes have a significantly lower risk.
- It is known that herpes viruses, during primary infection, incorporate their DNA into the genome of host lymphoid or nerve cells. In the latent phase of infection, viral replication in the ganglia is minimal, but weakening of immunological surveillance, especially of specific cellular immunity, can lead to reactivation of the latent infection, which is usually much less intense than primary infection.
Clinical picture
Development usually occurs within a few hours to a few days. CNS infliction can be clinically manifested either as a mild disease (aseptic meningitis) or more often as a serious disease state - encephalitis. Likewise, the beginning can be creeping or peracute.
- Prodromal symptoms include fatigue, fever (found in most patients), headache, nausea, vomiting.
- This symptomatology is followed by acute or subacute development of encephalopathy (behavioral disorders, lethargy or irritability, confusion, dysphasia, aphasia, photophobia), hemiparesis, cranial nerve deficits (paresis nn. VII., VI., III.), Visual field defects , paraesthesia, central limb paresis, vegetative disorders.
- Focal neurological findings and focal convulsions usually appear suddenly at the onset of the disease and persist for up to one week. We find focal convulsions in up to 40% of patients. Meningeal signs may be present, but are not common.
- In newborns and infants, we observe highly tuned crying, jaundice, respiratory distress, liver dysfunction.
- In older children, we can observe personality changes, behavioral disorders, memory changes, dysosmia, dysgeusia, hallucinations, bizarre ideas. These symptoms may appear early in the course of the disease and persist for about a week. They can often act as the onset of an acute psychiatric illness.
- In some patients, we observe a peracute course with progression of impaired consciousness leading to death without signs of focal neurological symptoms.
- Rare symptoms include the development of subacute encephalitis, which mimics psychiatric illness or benign recurrent meningitis. Rarely, HSV-1 can cause brainstem encephalitis, HSV-2 myelitis.
- In children who survived HSV encephalitis we may encounter severe antegrade amnesia (quickly forgotten learned) or severe retrograde amnesia (personal knowledge and orientation in time, interval even several years, some has poor memories of faces, many have language difficulties), there are also signs of frontal damage with behavioural disorders.
Diagnostics
When HSV encephalitis is suspected, diagnostic tests should be performed as soon as possible and we should never delay the start of therapy.
In the diagnosis of herpetic encephalitis, HSV cerebrospinal fluid PCR and CNS MRI have the highest yield!
- Basic laboratory tests are not helpful in diagnosing herpes infections, but they are essential because they can rule out other causes of the disease.
- Due to the symptomatology, a CT scan is often necessary in the introduction to rule out a focal lesion of a different etiology. In the diagnosis of HSV encephalitis, CT is evident after 3rd-4th the day of the disease, when it can detect necrotic changes in the temporal area. This option was used earlier, when earlier diagnosis was impossible, but always meant an ex post diagnosis.
- Today, it is replaced by early diagnostics using PCR and MRI.
- The cornerstone of diagnosis and examination are the lumbar puncture and cerebrospinal fluid examination. In the introduction we demonstrate a typical serous pattern with:
- mild elevation of proteinorrhea;
- normal glycorhachia;
- moderate pleiocytosis with a predominance of mononuclear cells.
- We can also find the presence of erythrocytes and xantochromatic appearance. Spectrophotometry eliminates artificial bleeding during the actual puncture.
- It is necessary to send cerebrospinal fluid for PCR detection of DNA for HSV-1 and HSV-2. HSV PCR is highly specific, with positivity remaining 5 days after initiation of acyclovir therapy. On the other hand, for the first 1-2 days and after two weeks of illness, the result may be false negative. The yield of cerebrospinal fluid examination is proportional to the amount of cerebrospinal fluid collected ("the more, the better"), we should usually obtain> 10 ml of cerebrospinal fluid. Despite the undeniable importance of PCR, it is necessary to realize that even this method does not have 100% sensitivity and specificity. In addition, the "quality" of the results varies according to the experience of the laboratories. Therefore, the diagnosis should always be made with regard to clinical symptomatology and further examination. False-negative results are rare, so many authors consider a negative HSV PCR result in the initial cerebrospinal fluid sample as sufficient evidence to discontinue acyclovir treatment.
- CSF antibody serology may support evidence of antibody response in the CNS.
- CT scan and MRI: MRI is more sensitive than CT and is now the imaging method of choice. In MRI we find most changes in the medial area of the temporal lobe and at the base of the frontal lobes, the lesions are often associated with cerebral edema, they are bilateral but rarely symmetrical. Gyrus deletion due to edema in the T1 image and high signal in the T2 image are considered to be early signs of the disease in the MRI image. After application of the contrast agent, enhancement may be found in the gyros. In neonatal HSV-2, we find panencephalitis.
- Another sensitive test for herpetic encephalitis is EEG. Indicates abnormality in 4/5 patients. We observe focal temporal changes and diffuse retardation of activity. Periodic high-voltage spikes - waves originating from the time domain and complexes of slow waves at 2-3 s intervals - are very telling for herpetic encephalitis. Normal EEG recording is rare, but does not rule out the presence of encephalitis.
- At some workplaces it is possible to perform tomographic isotope methodology using Tc - 99m = SPECT.
- Brain biopsy is an outdated diagnostic method.
Differential diagnostics
In addition to bacterial etiology (borrelia, leptospira) and encephalitis caused by other herpes viruses, it is necessary to exclude other possible agents such as:
We must rule out post-infectious and disseminated encephalomyelitis, which follows the viral disease - neurons are not directly infected with the virus, perivenous inflammation and demyelination located in the white matter are in the foreground (most common agents: EBV, CMV, HHV-6).
Cerebellitis (ataxia, tremor, vertigo, dysarthria, vomiting, fever) may occur in VZV infection approximately one week after rash.
Therapy
Patients with herpetic encephalitis should be treated and observed in the ICU. Base is:
- Thorough monitoring of vital functions.
- Early detection of convulsion (spasm) activity - seizures are very frequent during herpes encephalitis. We initiate anticonvulsant treatment without a clinical correlate if there is a specific finding on EEG. Commonly used benzodiazepines usually stop the spasm, but due to their short action they do not prevent recurrent seizures. Then a continuous administration of midazolam (eg) or a drug with a longer duration of action (barbiturates) is necessary.
- Early detection of an increase in intracranial pressure.
We provide patients with adequate nutrition and hydration according to their abilities (parenteral, nasogastric tube, orally). In case of proven intracranial hypertension, we initiate all necessary measures.
Causal medicine are antiviral drugs:
- acyclovir, (clearly preferred for higher efficacy and lower toxicity), at a dose of 20 mg/kg for adult i.v. every 8 hours in infusion for 21 days. Its side effects are minimal - renal dysfunction is described at high doses (therefore we do not administer acyclovir bolus).
- vidarabine
We should start acyclovir immediately after the possibility of herpetic encephalitis is suspected, we never wait with treatment for the confirmation of the infection. Afterwards, if HSV infection is not confirmed, acyclovir may be discontinued. Mortality was 60-70% before acyclovir treatment and 30% after it.
- In all neonates at the end of acyclovir treatment, we perform control lumbar puncture and re-examine HSV PCR. Its negativity is a requirement for the end of therapy. Subsequently, we switch to valaciclovir treatment in p.o. form for months to years. Valaciclovir (Valtrex) after p.o. administration converts rapidly to acyclovir. It is more expensive, but compared to p.o. acyclovir has better bioavailability.
- Adequate rehabilitation is also a part of comprehensive treatment.
Complications
The most common consequences in surviving patients are:
- motor deficits;
- secondary epilepsy syndrome;
- change in mental state.
The consequences are more frequent in patients with delayed treatment. Patients who started treatment within 5 days of the first symptoms have better results. Interestingly, both HSV-1 and HSV-2 have comparable mortality, but HSV-2 has higher morbidity, ie more frequent neurological consequences (motor deficits, convulsions, microcephaly, sight defects). Subsequent psychiatric changes (hypomania, various degrees of amnesia, Klüver-Bucy syndrome), recurrent aseptic meningitis - Mollaret's meningitis are also reported in connection with herpes encephalitis.
Mollaret's meningitis
It is a recurrent benign aseptic meningitis. Headaches, meningeal symptoms and fever are typical, and neurological symptoms are only transient. In the cerebrospinal fluid we find mixed pleiocytosis with mononuclear cells, polynuclear cells, endothelial cells (Mollaret cells) and elevated gammaglobulins. PCR can detect HSV-2, uncommonly also EBV or enteroviruses. The therapy is only symptomatic, as the symptomatology disappears spontaneously within a few days. Prophylactic administration of acyclovir or valaciclovir may prevent attacks.
Links
Source
- MUDr.HAVRÁNEK, Jiří: Herpetická meningoencefalitida
Similar articles
Herpes zoster
Varicella zoster virus (VZV) causes clinically 2 different diseases:
- Chickenpox (Varicella)
- Shingles
VZV causes common encephalitis, rarely acute disseminated encephalitis.
Patogenesis
The virus survives in the latent form in the sensitive ganglia of the posterior spinal roots: ganglion Gasseri (nervus trigeminus) and ganglion geniculi. The infection ignites when the body is weakened (surgery, general illness, etc.). The infection usually spreads to the periphery in the respective skin dermatome.
Clinical findings
During the dermatome, pain appears, sometimes preceded by itching. In a few days, a serous (even partially hemorrhagic) rash of various magnitudes appears, and the regional lymph nodes are painful and swollen. The blisters dry out after 2 weeks, leaving depigmentation or hyperpigmentation, the pain gradually disappears. In some patients, severe neuralgic pain persists in the respective dermatome even after the crust separates. Paresis are present in 20% of the cases, encephalitis is rare.
- Herpes zoster oticus
When the ganglion geniculi is affected. The blisters appear in the ear canal and around the ear itself. Hunt's syndrome - hearing impairment, dizziness, paresis of the facial nerve (n. VII).
- Herpes zoster ophthalmicus
Gasseri ganglion lesion. Sowing of blisters in the first branch of the trigeminal nerve (ophthalmic nerve). It causes conjunctivitis and the risk of keratitis. 50-70% of patients have eye complications. It occurs predominantly at an older age (in the 5th-8th decade). We find an increase of lymphocytes in the cerebrospinal fluid.
Treatment
The drug of choice is aciclovir. Descending treatment of prednisone. Also liquid powder for the treatment of the blisters, ATB against superinfection and for neuralgia carbamazepine or tricyclic antidepressants.
Vaccination
Zostavax live vaccine is indicated for people over 50 years of age. After undergoing shingles, an interval of 6 months is recommended. Contraindicated in pregnant, immunosuppressed, active untreated TB, hypersensitivity to vaccine components. Available in the Czech Republic since 2014, it is not covered by health insurance.
Links
References
- SEIDL, Zdeněk a Jiří OBENBERGER. Neurologie pro studium i praxi. 1. vydání. Praha : Grada Publishing, 2004. ISBN 80-247-0623-7.
- ↑ Medixa - Herpes zoster
- ↑ TOPINKOVÁ, Eva. Herpes zoster a očkování proti němu [online]. www.ProLékaře.cz, ©2014. [cit. 30. 10. 2014]. <https://www.prolekare.cz/preventabilni-onemocneni-novinky/herpes-zoster-a-ockovani-proti-nemu-4256,>.
Source
Rabies (rabies, lyssa)
Rabies (lyssa) is a viral infectious disease that spreads from wild and domestic animals. Once clinical symptoms break out, the disease is always fatal.
The Czech Republic has been considered "Rabies-free" since 2004 (rabies does not occur in the Czech Republic). In the Czech Republic, you can find imported rabies or rabies after a bat bite. There is an increased risk of rabies at the borders with Poland and Slovakia (these countries are not "Rabies-free").
Patogeneze
- Primární encefalitida způsobená lyssavirem, patřící do skupiny Rhabdoviridae,
- přenáší se slinami zvířete při pokousání či infikovaným škrábnutím,
- virus se z místa kontaminace do CNS šíří perineurálně,
- o délce inkubace rozhoduje vzdálenost poranění od hlavy (2 týdny až několik měsíců).
Patologicko-anatomický obraz
- V cytoplazmě napadených buněk inkluzní Negriho tělíska,
- virus napadá kůru mozkovou, oblongatu, jádra hlavových nervů a spinální ganglia.
Klinické příznaky
- Po inkubaci se objeví nespecifické příznaky – zvýšená únavnost, emoční labilita, poruchy spánku, napětí v jizvě,
- posléze paroxyzmy křečí – faryngospasmy s dysfágií, hydrofobie,
- profúzní salivace a pocení,
- smrt za pár dní za příznaků hyperpyrexie a selhání srdce.
Diferenciální diagnostika
Diferenciálně diagnosticky je nutné odlišit tetanus.
Léčba
Léčba vztekliny neexistuje.
Profylaxe
Nutné je nechat vyšetřit zvíře veterinářem. Při kousnutí infikovaným zvířetem nebo zvířetem s rizikem vztekliny je nutná tzv. postexpoziční profylace. Jedná se o kombinaci aktivní (vakcína) a pasivní (antirabické heterologní koňské sérum) imunizace. Vakcína se podává v 5 dávkách ve schématu 0-3-7-14-28. U cestovatelů a veterinářů je možná i preexpoziční profylaxe.
Reyův syndrom
Poliomyelitis anterior acuta (Heineova-Medinova nemoc, dětská obrna)
__
Poliomyelitis anterior acute, also known as polio (transmissible) or Heine-Medin disease, is an epidemic summer virus. It is caused by the non-enveloped ssRNA Poliovirus from the genus Picornaviridae. Poliovirus has 3 antigenic types without crossimmunity.
Given that anterior acute poliomyelitis has already been eradicated in the Czech Republic, it is possible to encounter so-called polio-like syndromes or poliomyelitis acquired abroad. "Polio-like syndromes" are manifested by peripheral paresis and muscle atrophy in the area of one or two joints. Sensory disturbances are not usually present, but pain may occur. EMG shows signs of an acute motoneuron lesion.[5]
Features
The course of the disease is often silent and is limited to the gastrointestinal tract - water and food can be contaminated this way. It is transmitted through the patient's stool. It selectively affects the frontal horns of the spinal cord' and the motor nuclei of the trunk. It has the same clinical picture as echoviruses and Coxsackie viruses.
Epidemiology
In Czechoslovakia, the incidence has been zero since 1957 (we are the first country in the world to do so). Poliovirus has 3 antigenic types – I, II, III' and man is the only natural host of virusu. Viremia and penetration into the CNS will only occur in a small percentage.
- Eradication[6]
We divide the regions into:
- endemic: Afghanistan, Nigeria, Pakistan,
- and non-endemic: Central African Republic, Chad, Ivory Coast, Democratic Republic of Congo, Ethiopia, Israel, West Bank, Gaza Strip, Kenya, Liberia, Mali, Niger, Somalia, Uganda. [7]
The European region was declared polio-free in June 2005. The risk of importation of poliomyelitis is still looming.
- WHO Polio Eradication Program[6]
- Virological examination of patients with weak paresis.
- Investigation of contacts.
- Compulsory reporting.
- Expert analysis of isolates.
Pathology
Infiltration of lymphocytes and granulocytes around stem motor nuclei and anterior horn cells spinal. Proliferation of microglia.
Clinical symptoms
Incubation period: 5-14 days' [1]. flu symptoms appear - fatigue, temperature, sweating, headache, digestive problems. What follows is healing'.
Only a fraction progresses to meningitis → headache, back pain, limb pain, meningeal symptoms, muscle stiffness = preanalytical stage'' (or meningeal). In about 2% it progresses in the nervous system = paralytic stage.
The course is most often ``asymptomatic. All stages leave an immunity' to the virus. The spread of the virus is aided by its excretion in the stool (3 months after the infection subsides).
- Spinal form
Affects the front (sometimes lateral) horns of the spinal cord. There are muscle fasciculations and paini. Paresis and vegetative manifestations develop within 24 hours. It can also affect the respiratory muscles.
- Stem form
It leads to paresis of the pharynx, larynx, tongue, and facial expressions with possible spread to the respiratory muscles and the heart. Improvement occurs as early as a week after the development of nerve symptoms and continues up to 1 year. It leaves serious lasting effects'. Residual peripheral paresis affecting various muscle groups of the limbs and trunk, muscle contractures.
Diagnosis
- Clinical picture + examination of CSF (cytoprotein association).
- Virus isolation from stool, rise of specific antibodies in cerebrospinal fluid and serum (confirmation of diagnosis).
Differential diagnosis
Other acute meningitis, polyradiculoneuritis, transverse myelitis.
Treatment and Prevention
In the acute phase of the disease, physical rest and drinking regimen are the most important. In severe forms (ascending Landry's palsy), intensive care is needed (UPV - mainly negative pressure ventilation, using the so-called iron lung). It is a continuous long-term process. Interdisciplinary medical cooperation and parental cooperation are important.
Prevention
Mortality reached up to 25% in the epidemic, the last one in our country in 1960. A fundamental change was brought about by the introduction of active immunization in 1957, when vaccination with inactivated (Salk) vaccine began. Since 1960, vaccination with the ``oral live vaccine (Sabin) has been started.
Since 2007, based on WHO recommendations, the Czech Republic has again been vaccinated with an "inactivated" vaccine, which is administered as part of a "hexavaccine" or as a "monovaccine" in five doses. The reason for switching to an inactivated vaccine is the fact that when using it, the virus is not excreted in the stool or the virus mutates, so there is no risk of post-vaccination poliomyelitis.[8]
Prognosis
Good for all forms except paralytic. Lethality of the paralytic form is 5-15%', survivors no longer recover. Unusual fatigue, joint and muscle pain, further weakening of the muscles, probably due to overloading of functioning muscle groups.
Preference is given to placing the child in a normal group. Another option is the Jedličk Institute in Prague.
Post-polio syndrome
Usually during the 20 years of peace after stabilization of the clinical residue after the paralytic form of poliomyelitis. The cause is overload and dysfunction of the remaining motoneurons of the anterior horns of the spinal cord.
Symptoms: increased fatigue, muscle weakness (even in previously unaffected segments), fasciculation, pain in affected muscles and joints.
Therapy: non-specific, includes supportive orthoses and gentle rehabilitation.
Syndrom získané imunodeficience (AIDS)
thumb|Mikroskopie Kaposiho sarkomu. Toto onemocnění známé od roku 1981[1]působí retrovirus HIV. Neuro- a lymfotropní vlastnosti umožňují viru invazi do CNS, stejně jako progresivní destrukci imunitního systému (ničí T4 lymfocyty). Přenáší se horizontálně (pohlavní styk, krevní deriváty, parenterální aplikace drog) nebo vertikálně (z matky na dítě). Skupiny, které jsou rizikovější k námaze, jsou například homosexuálové, narkomani, hemofilici nebo děti infikovaných matek.
Klinické příznaky
Akutní infekci uvádí horečka a zdruření uzlin. Protilátky proti HIV se objeví nejdříve za 1–3 měsíce[1] a jejich pozitivita je jediným projevem až u 70 % nakažených[1] Toto stadium symptomatické chronické infekce může trvat měsíce až roky. Nemocní mají často příznaky, které nazýváme komplex spojený s AIDS (ARC), do kterého patří průjmy, letargie, hubnutí, oportunní infekce (kandidóza, impetigo). HIV pozitivitu také provází lymfopenie, trombocytopenie. AIDS znamená progresi k těžkým oportunním infekcím a tumorům, jako například:
- pneumocystová pneumonie (50 %),
- Kaposiho sarkom (20 %), lymfom CNS,
- non-Hodgkinské lymfomy,
- tuberkulóza.
Neurologické projevy se vyskytují u 80 % nemocných[1], jejich nástup má vazbu na sérokonverzi a na pozdní AIDS.
Léčba
Léčbu je třeba nasadit okamžitě, při podezření na mozkovou toxoplasmózu podáváme pyrimethamin nebo sulfadiazin. Pokud se CT obraz nelepší, indikujeme biopsii (lymfom). AIDS končí nevyhnutelně fatální infekcí či malignitou. Zkouší se také léky mobilizující imunitní systém a ovlivňující replikaci viru, jako zidovudin (AZT), který blokuje tvorbu HIV specifické DNA a tak omezuje replikaci viru. Při terapii používáme také imunomodulátory, jako např. IFN, IL–2.
Subakutní sklerózující panencefalitida
__ Subakutní sklerózující panencefalitida
Progresivní multifokální leukoencefalopatie
__ Progresivní multifokální leukoencefalopatie
Odkazy
Související články
Reference
- ↑ Jump up to: a b c d e f Cite error: Invalid
<ref>tag; name "Seidel" defined multiple times with different content - ↑ Jump up to: a b VOKSHOOR, A a C WAN. https://emedicine.medscape.com/ [online]. ©2007. [cit. 2.7.2009]. <https://emedicine.medscape.com//article/1168529-overview>.
- ↑ SEIDL, Zdeněk a Jiří OBENBERGER. Neurologie pro studium i praxi. 1. vydání. Praha : Grada Publishing, 2004. ISBN 80-247-0623-7.
- ↑ SEIDL, Zdeněk a Jiří OBENBERGER. Neurologie pro studium i praxi. 1. vydání. Praha : Grada Publishing, 2004. ISBN 80-247-0623-7.
- ↑ EHLER, E – DERĎÁKOVÁ, M – LATTA, J. , et al. Akutní polyradikuloneuritida – diferenciální diagnostika. Neurológia pre prax [online]. 2011, y. 12, p. 180-181, Available from <http://www.solen.sk/index.php?page=pdf_view&pdf_id=5109>.
- ↑ Jump up to: a b ŽAMPACHOVÁ, Eva. Přednášky a materiály dr. Žampachové ke stažení [online]. [cit. 2012-01-27]. <http://mujweb.cz/?redirected=1521314685>.
- ↑ WHO. The Global Polio Eradication Initiative - Infected countries [online]. [cit. 2013-10-26]. <http://polioeradication.org/Infectedcountries/Importationcountries/Israel,WestBankandGaza.aspx>.
- ↑ STAŇKOVÁ, Marie – VANIŠTA, Jiří. Medicabáze.cz – Poliomyelitida [online]. ©2008. [cit. 6. 2. 2010]. <http://medicabaze.cz/?&sec=term_detail&termId=1619&tname=Poliomyelitida>.
Kategorie:Neurologie
Kategorie:Mikrobiologie
Kategorie:Viry
Kategorie:Infekční lékařství