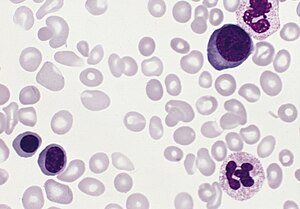
Diseases caused by increased number of erythrocytes
|
This article was marked by its author as Under construction, but the last edit is older than 30 days. If you want to edit this page, please try to contact its author first (you fill find him in the history). Watch the discussion as well. If the author will not continue in work, remove the template Last update: Thursday, 12 Nov 2020 at 4.46 pm. |
Polycythaemia vera
Polycythaemia vera (PV, primary polycythaemia, Vaquez's disease) is a disease with a high number of erythrocytes + high concentration of Hb → increases blood viscosity + arterial thrombotisation (cause of death is thrombosis of coronary + cerebral arteries ).
Pathogenesis
- Clonal proliferation of a pluripotent hematopoietic stem cell, kt. differentiates mainly into the erythrocyte line;
- increased sensitivity of BFU-E progenitors to the effects of erythropoietin;
- the possibility of differentiation into erythroid precursors even without erythropoietin;
- there is also a slight increase in bb. other rows.
Clinical picture
- Headache , dizziness , etc.,
- digestive problems, frequent Gastroduodenal ulcer disease ,
- pruritus,
- frequent bleeding / conversely arterial and venous thrombotic events, incl. coronary artery obliteration,
- Arthritis uratica (gout),
- brownishness, cyanosis ,
- splenomegaly (in advanced stages up to the pelvis).
Diagnostics a diff. dg.
- Increased value of Hb + HTK (50-70%),
- can be masked if plasma is also increased;
- there may be leukocytosis + a slight shift to the left,
- often also thrombocytosis,
- blood oxygen saturation < 92% can be the cause of secondary polyglobulia ,
- low ferritin values more common in primary polycythemia than in secondary polyglobulia; concentration of vitamin B12 + its binding capacity increased, conc. folate reduced,
- in PV, the concentration of endogenous erythropoetin is reduced,
- the histological height is essential. bone marrow (PV image different from reactive polyglobuli) + molecular-biological examination,
- dg. PV rests hl. in the detection of general signs of myeloproliferative disease, in the case of embarrassment to exclude a secondary cause (difficult),
- frequent thrombotic/bleeding events (in patients with secondary polyglobulia few).
Therapy
- Medical venipuncture , erythrocytapheresis (more expensive, exceptionally),
- IFN-α ,
- hydroxyurea,
- anagrelide + therapeutic venipuncture in patients resistant to IFN + hydroxyurea,
- treatment of pruritus + hyperuricemia .
Prognosis
- Average survival 15 years,
- cause of death: thrombosis, acute leukemia , other cancer, bleeding , etc.[1][2]
Summary video
Secondary polyglobulia
Secondary polyglobulia is mostly compensatory in chronic hypoxia (leads to ↑ EPO) when staying at high altitude, chronic lung disease, right-to-left shunts, methemoglobinaemia.
Less often, the cause of ↑ EPO is unclear/a manifestation of a disease (kidney tumors, uterine myomatosis, polycystic kidney disease, etc.).
The clinical picture
- mainly symptoms of underlying lung/heart disease,
- plethoric appearance, cyanosis,
- headaches, dizziness, visual disturbances.
Laboratory Tests
- ↑ erythrocytes, HTK > 48%, oxygen saturation <92%, ↑ EPO (dif. dg. Polycytaemia vera).
Therapy
- Th. of underlying disease, venipuncture (↓ blood viscosity + reduces the risk of complications).[3]
Erythrocytosis
False polyglobulia is caused by a decrease in volume of plasma, total erythrocyte volume is normal:
- Stress polycythemia in young people (+ hypertension, obesity = Gaisböck's syndrome)
- Relative polyglobulias in dehydration, extensive burns, etc.
Neonatal polycythemia
Neonatal polycythemia is defined as a central venous hematocrit > 0,65. Nowever, even with a hematocrit> 0.70, only a small proportion of neonates have clinical signs of hyperviscosity. The clinical picture includes lethargy, hypotension, hyperbilirubinemia and hypoglycemia. Polycythemia may also be involved in the development of convulsions, stroke, renal venous thrombosis and necrotizing eneterocolitis.
Causes of neonatal polycythemia:
- Fetal growth restriction (FGR, IUGR);
- maternal hypertension;
- maternal diabetes;
- chromosomal defects: trisomy 21, 18, 13;
- twin-to-twin transfusion;
- delayed umbilical cord rupture;
- endocrine disorders: tyreotoxicosis, congenital adrenal hyperplasia (CAH).
Treatment is controversial and may not be necessary in neonates with mild symptoms (eg borderline glycaemia, impaired peripheral blood flow). Treatment is indicated in neonates with a hematocrit> 0.65 and symptoms with a potentially severe prognosis (eg refractory hypoglycaemia, neurological symptoms). A partial exchange transfusion is performed with a crystalloid solution (eg physiological solution) with a target hematocrit of 0.55.[4]
Links
Related articles
Reference
- ↑ NEČAS, Emanuel. Patologická fyziologie orgánových systémů : Část I. 2. edition. V Praze : Karolinum, 2009. 379 pp. ISBN 978-80-246-1711-4.
- ↑ DÍTĚ, P.. Vnitřní lékařství. 2. edition. Praha : Galén, 2007. ISBN 978-80-7262-496-6.
- ↑ KLENER, P. Vnitřní lékařství. 3. edition. Galén, 2006. ISBN 80-7262-430-X.
- ↑
Template:Navbox - onemocnění krve